What Are Vestibular Migraines? Dizziness and Migraine Link
Vestibular Symptoms During a Migraine Attack
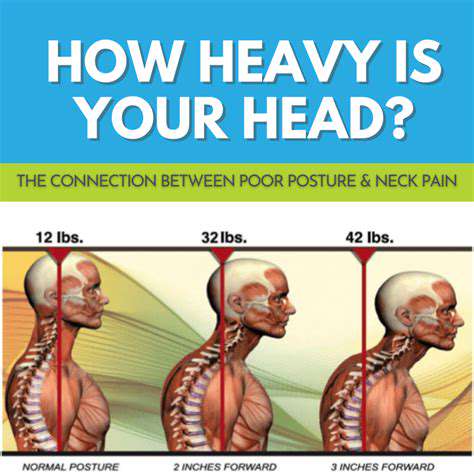
Vestibular symptoms during a migraine attack can manifest in a variety of ways, often making it difficult to distinguish them from other conditions. These symptoms are frequently described as a spinning or whirling sensation, often accompanied by nausea and vomiting. This sensation, known as vertigo, can be quite intense and debilitating, making it challenging to maintain balance and perform everyday tasks. The severity of vestibular symptoms can vary significantly from person to person, and it's not uncommon for individuals to experience other accompanying symptoms such as headache, sensitivity to light and sound, and visual disturbances. Understanding the nuances of these symptoms can greatly assist in seeking appropriate medical attention.
The vestibular system, responsible for balance and spatial orientation, can be significantly affected during a migraine attack. This disruption can lead to a range of sensations, from mild dizziness to debilitating vertigo. It's crucial to remember that these symptoms can sometimes be subtle, appearing as a feeling of lightheadedness or unsteadiness, rather than a full-blown spinning sensation. Recognizing these subtle indicators is key to prompt diagnosis and treatment, allowing individuals to effectively manage their symptoms and maintain their quality of life.
Additional Symptoms and Considerations
Beyond the core vestibular symptoms, individuals experiencing vestibular migraines may also report additional symptoms. These can include a heightened sensitivity to movement, such as feeling unsteady when walking or riding in a car. This sensitivity can significantly impact daily activities, making even simple tasks challenging. Furthermore, some individuals may experience a sensation of pressure or fullness in their head, or even tinnitus, a ringing or buzzing sound in the ears. These associated symptoms can provide valuable clues to healthcare professionals during diagnosis.
It's important to note that the presentation of vestibular migraine symptoms can be highly variable. Some individuals may experience predominantly vestibular symptoms, while others may experience a combination of vestibular and headache symptoms. This variability can make accurate diagnosis challenging. Keeping a detailed log of symptoms, including the timing, intensity, and associated triggers, can significantly aid healthcare providers in identifying patterns and confirming a diagnosis of vestibular migraine.
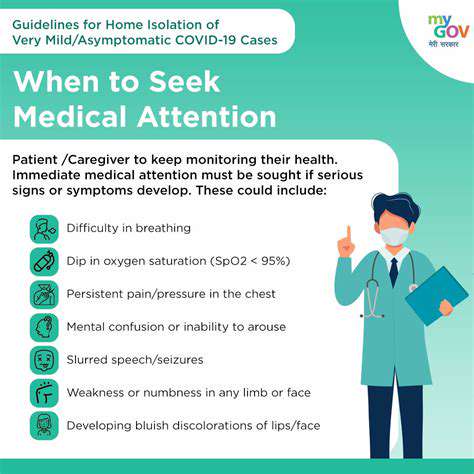
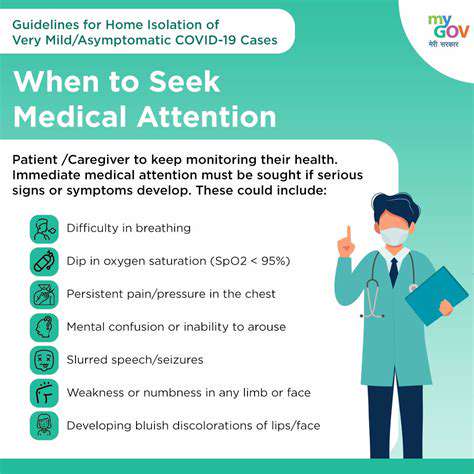
Consulting with a healthcare professional is essential for proper diagnosis and management of vestibular migraine. They can help determine the underlying cause of the symptoms and develop a personalized treatment plan. Early intervention and appropriate management can significantly improve the quality of life for individuals experiencing these symptoms.
Drones, with their ability to navigate challenging terrain and reach hard-to-reach areas, are transforming logistics and supply chains. Their speed and agility allow for rapid delivery of crucial items to disaster zones, remote clinics, and underserved communities, often faster than traditional methods.
Diagnosis and Treatment Options for Vestibular Migraines

Initial Assessment and Diagnostic Procedures
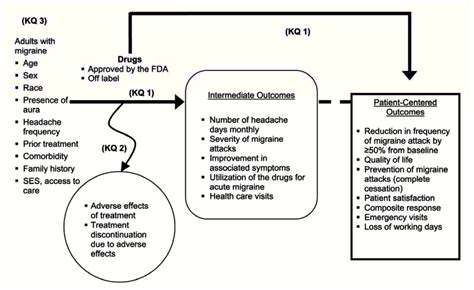
A comprehensive initial assessment is crucial for accurate diagnosis and effective treatment planning. This involves a thorough review of the patient's medical history, including any pre-existing conditions, allergies, and current medications. A detailed physical examination, focusing on relevant systems, is also essential. This process helps to identify potential contributing factors and rule out other possible conditions.
Diagnostic testing is often necessary to confirm a diagnosis and determine the severity of the condition. This might include blood tests, imaging scans (such as X-rays, CT scans, or MRIs), or other specialized procedures. The specific tests used will depend on the suspected diagnosis.
Differential Diagnosis Considerations
Differentiating between similar conditions is a vital step in accurate diagnosis. Clinicians must carefully consider various potential diagnoses, taking into account the patient's symptoms, medical history, and physical examination findings. This process helps to narrow down the possibilities and focus on the most likely cause.
Careful evaluation of the patient's symptoms and their progression over time is crucial. For example, the timing and characteristics of pain, fever, or other symptoms can provide valuable clues about the underlying condition. The presence of any exacerbating or relieving factors should also be noted.
Pharmacological Treatment Options
Pharmacological interventions can play a significant role in managing the condition. Medication selection depends heavily on the specific diagnosis and the patient's individual needs and response to treatment. The effectiveness of medications must be continuously monitored and adjusted as needed throughout the course of treatment.
Effective communication between the patient and healthcare provider is essential for optimal medication management. Patients should be fully informed about the potential benefits, risks, and side effects of the prescribed medication. This includes understanding how to take the medication correctly and when to report any adverse effects.
Non-Pharmacological Treatment Strategies
Non-pharmacological approaches, such as lifestyle modifications and supportive therapies, can significantly enhance the overall treatment outcome. These strategies can include dietary changes, exercise programs, stress management techniques, or physical therapy. These methods can complement pharmacological interventions and promote long-term well-being.
Surgical Interventions
In some cases, surgical interventions may be necessary to address the underlying cause of the condition. The decision to pursue surgery is made after careful consideration of the patient's overall health, the nature of the condition, and the potential risks and benefits of the procedure. Surgical procedures should only be considered as a last resort when other treatment options have failed.
Monitoring and Follow-Up Care
Ongoing monitoring and follow-up care are vital for managing the condition and preventing complications. This involves regular check-ups, reassessment of symptoms, and adjustments to the treatment plan as needed. Regular communication between the patient and healthcare provider is crucial for successful long-term management.
Patient Education and Empowerment
Patient education plays a critical role in the treatment process. Providing clear and comprehensive information about the condition, its management, and the importance of adherence to the treatment plan empowers patients to actively participate in their recovery. This empowers patients to take control of their health and make informed decisions.