Middle of Head Hurts: Possible Causes and Treatment Options
A Complete Guide to Headache Types and Coping Strategies
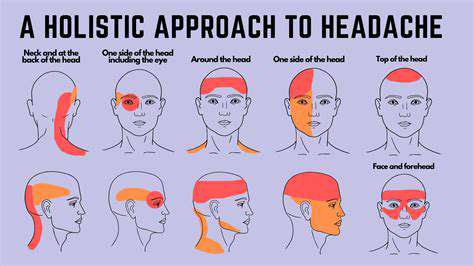
Tension-type headaches are common and mild, often presenting as a dull ache in the head.
During migraine attacks, they are accompanied by nausea and light sensitivity, with significant pain intensity.
Central headaches caused by sinusitis are often accompanied by nasal congestion and runny nose symptoms.
Cluster headaches present a characteristic of periodic severe pain.
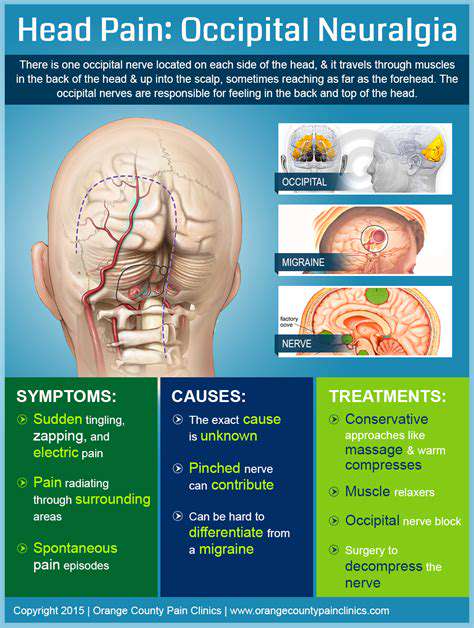
Cervicogenic headaches are closely related to cervical spine issues.
Hypertension may lead to increased intracranial pressure, causing headaches.
Accurately identifying headache types is the foundation for developing treatment plans.
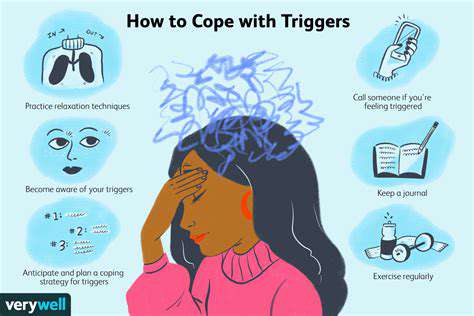
Stress, food allergens, and environmental irritants are potential triggers.
Different management strategies are required for acute episodes versus chronic pain.
Medication therapy must distinguish between analgesic and preventive types.
Non-drug interventions like cognitive behavioral therapy have significant effects.
Regular exercise and hydration are basic preventive measures.
Worsening persistent headaches require timely professional medical help.
Regular health check-ups help track headache patterns and health risks.
1. Common Causes of Central Headaches
1.1 Tension-type Headaches
Tension-type headaches are the most common type, often presenting as a pressure-like dull pain from the forehead to the crown of the head. Clinical data shows that about 80% of adults have experienced this type of headache, which is directly associated with muscle tension, accumulation of stress, or poor posture.
It is worth noting that this type of headache often accompanies scalp tenderness and shoulder and neck stiffness, forming complex discomfort symptoms. Utilizing soothing exercises such as yoga combined with mindfulness meditation can effectively reduce the frequency of attacks. It is recommended to set up ergonomic seating in work areas and perform neck and shoulder stretching every 45 minutes of work.
1.2 Migraines
Migraine patients often describe the pain as pulsating and concentrated in the crown area, affecting about 12% of the population, with female incidence being three times that of males. Typical attacks may last 4-72 hours, with about one-third of patients experiencing visual aura symptoms.
It is crucial to record dietary, sleep, and stress levels during attacks. Clinical findings indicate that certain cheeses and the tyramine component in red wine may trigger attacks; maintaining a regular routine and recognizing individual triggers is key to management. Newly developed CGRP inhibitors offer new options for stubborn cases.
1.3 Sinusitis Headaches
When the maxillary or ethmoid sinuses become inflamed, nasal congestion leads to typical pressure pain between the eyebrows. Among the more than 30 million sinusitis cases in the U.S. each year, about 65% accompany headache symptoms. Increased pain upon waking is an important judgment criterion for this type.
Using saline nasal irrigation and steam inhalation can effectively alleviate symptoms. It should be noted that symptoms persisting for more than 10 days may indicate a bacterial infection, requiring antibiotic treatment. Maintaining environmental humidity at 40-60% can prevent mucosal dryness.
1.4 Cluster Headaches
Cluster headaches, referred to by patients as suicide headaches, have a pain intensity that can match childbirth. The incidence in males is three times that of females, typically presenting as knife-like pain around one eye, often occurring at regular times during the night.
High-flow pure oxygen inhalation can relieve 80% of acute attacks within 15 minutes. Preventative medications such as verapamil can reduce annual attack frequency by 70%. Interestingly, some patients report that capsaicin nasal spray can block pain signal transmission.
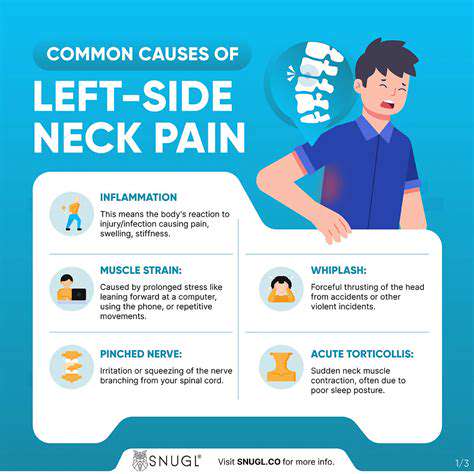
1.5 Cervicogenic Headaches
This type of headache originates from cervical joint dysfunction or muscle strain, with pain radiating from the back of the head to the forehead. Technology neck caused by prolonged use of electronic devices is a significant trigger, with about 22% of chronic headaches belonging to this category.
Targeted cervical stability training has shown significant effects. Clinical studies indicate that biweekly deep muscle strengthening training for the neck, combined with heat therapy, can reduce pain scores by an average of 58% after three months. Adjusting the computer screen to eye level can reduce neck pressure by 40%.
1.6 Other Potential Triggers
Hypertensive crises (≥180/120 mmHg) can trigger thunderclap headaches, which fall under emergency conditions. Some antidepressants and nitrate medications may also lead to medication-overuse headaches, with symptoms usually alleviating after dose adjustment.
Keeping a headache diary to record the timing, intensity, accompanying symptoms, and medications is recommended. When changes in consciousness, double vision, or limb numbness occur, immediate medical attention is required for CT or MRI to rule out organic diseases.
2. Symptoms Recognition and Trigger Tracking Techniques
2.1 Symptom Feature Analysis
- Pain Nature: Dull pain, throbbing pain, and sharp pain need to be distinguished.
- Accompanying Symptoms: Light and sound sensitivity hints at migraines, while runny nose and congestion point to sinusitis.
- Temporal Patterns: Worsening in the morning may be related to sleep apnea.
It is recommended to use a VAS (Visual Analog Scale) to quantify pain intensity. For example, use a 0-10 scoring system; if the score persists at ≥5 for more than three days, consideration should be given to adjusting the treatment plan. Smell sensitivity testing can help differentiate migraine subtypes.
2.2 Trigger Screening Methods
Utilize an exclusion method to gradually screen potential triggers: first, adjust the sleep cycle to 7-9 hours/day and observe changes over two weeks; next, keep a dietary diary, especially watching for common triggers like nitrites (processed meats), monosodium glutamate (MSG), and artificial sweeteners.
Barometric pressure changes are often overlooked triggers; using a barometer app can track the correlation between weather systems and headache episodes. It is advisable for susceptible individuals to perform preventive hydration and magnesium supplementation 24 hours before significant weather changes.
3. Comprehensive Analysis of Headache Management Plans
3.1 Stepwise Medication Principles
Acute treatment should follow a two-step principle: first-line choices include NSAIDs such as ibuprofen; if ineffective, escalate to triptans. It is important to note that using analgesics more than 15 days monthly may lead to medication-overuse headaches.
For preventive medications, propranolol and amitriptyline have an efficacy of about 60%, and new anti-CGRP monoclonal antibodies can reduce the number of migraine days per month by 50%. It is advisable to combine magnesium (400mg/day) and coenzyme Q10 (300mg/day) as basic nutritional support.
3.2 Non-Drug Intervention Systems
Biofeedback therapy trains relaxation techniques by monitoring electromyographic signals, with clinical data showing a 45% reduction in tension-type headache attacks. Performing aerobic exercises three times a week along with breathing training can improve pain thresholds by 30%.
Cognitive Behavioral Therapy (CBT) is highly effective for chronic headaches, changing pain cognition patterns with 60% of patients showing declines in pain-related functional disability indices after a 12-week program. Combining this with progressive muscle relaxation training, twice daily for 20 minutes each time, is recommended.
4. Judging the Timing for Medical Intervention

4.1 Warning Sign Recognition
When headaches present as sudden, lightning-like extreme pain (peaking within 1 minute), or are accompanied by fever and neck stiffness, immediate exclusion of subarachnoid hemorrhage or meningitis is necessary. New headaches in individuals over 50 should raise suspicion of giant cell arteritis.
Emergency evaluation is recommended for the following situations:
- Pain worsens with coughing/straining
- Signs of neurological deficits (double vision, unsteady gait)
- New headaches in cancer/HIV patients
4.2 Chronic Disease Management Strategies
Chronic headache patients are advised to monitor blood pressure and undergo fundus examinations quarterly. For chronic migraines occurring more than eight times a month, consideration can be given to type A botulinum toxin injections, which block pain signal transmission and reduce headache days by 50%.
Establishing a headache management file to record medication responses and side effects is recommended. When there is a decrease in medication effectiveness, timely adjustments should be made rather than self-increasing the dosage. A multidisciplinary treatment model integrating neurology, rehabilitation, and psychological consultation can improve treatment outcomes by 35%.