What Really Causes Migraines? Exploring the Science

Environmental Triggers and Mental Health
Our surroundings profoundly influence psychological states, with pollution, noise, and extreme weather events acting as invisible stressors. These elements don't just affect our physical spaces - they reshape our neural pathways, potentially leading to anxiety disorders or depressive episodes. The science behind this environmental-mental health connection reveals fascinating neurobiological mechanisms worth exploring.
When hurricanes displace communities or wildfires destroy neighborhoods, the psychological aftermath often outweighs the physical damage. Survivors frequently describe losing their sense of safety and stability, with some developing PTSD symptoms months after the event. This demonstrates how environmental crises become mental health emergencies requiring specialized care.
The Social Environment's Powerful Influence
Human interactions create an invisible ecosystem that nurtures or poisons mental health. Workplace bullying, racial discrimination, or social exclusion don't just hurt feelings - they trigger measurable stress responses that accumulate over time. Positive social connections function like psychological airbags, softening life's impacts, while toxic relationships act like constant background radiation.
Interestingly, social media platforms have created hybrid environments blending digital and physical spaces. These platforms amplify certain social triggers while muting others, creating novel mental health challenges researchers are just beginning to understand.
Urban Design's Psychological Footprint
City planners rarely consider the mental health implications of concrete jungles versus green spaces. Yet studies show hospital patients with park views recover faster, and office workers near windows report better mood. The reverse proves equally true - cramped, noisy, polluted urban areas correlate with higher anxiety medication prescriptions.
Singapore's biophilic design initiative demonstrates how intentional urban planning can combat stress. By mandating green roofs, vertical gardens, and accessible parks, they've created an urban environment that actively supports mental wellness rather than undermining it.
Multidimensional Solutions for Complex Problems
Combating environmental triggers requires equal parts policy change and personal adaptation. While governments must regulate pollution and fund green spaces, individuals can cultivate micro-habits like forest bathing or creating social support networks. The most effective interventions acknowledge both systemic and personal factors, offering tools to navigate unavoidable stressors while working to eliminate preventable ones.
Emerging technologies like VR nature experiences and noise-canceling urban architecture hint at future solutions. Meanwhile, simple present-day actions - planting community gardens or establishing neighborhood watch programs - demonstrate how small environmental tweaks can yield significant mental health dividends.

Current Research and Future Directions
Decoding the Brain's Chemical Language
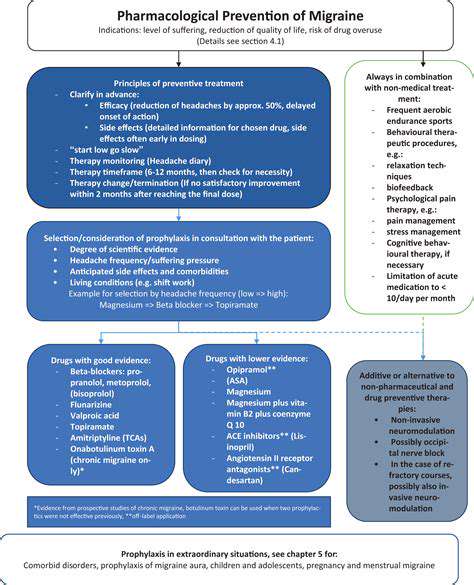
Neuroscientists now view migraines as neurological storms where serotonin and glutamate act like misbehaving conductors. Advanced imaging reveals how these chemical imbalances create chain reactions - first hypersensitizing neurons, then amplifying pain signals until normal sensations become unbearable. Pharmaceutical research focuses on developing smarter medications that target specific receptors without causing systemic side effects.
Nature vs. Nurture in Headache Science
Family migraine patterns suggest genetic components, but identical twin studies reveal environment's crucial role. Researchers now map how specific genes increase vulnerability to certain triggers - explaining why one person gets headaches from barometric pressure changes while another reacts to hormonal shifts. This knowledge fuels personalized prevention strategies moving beyond one-size-fits-all approaches.
The Inflammation Connection
Cutting-edge studies show migraine brains in flare-up mode, with inflammatory markers resembling miniature versions of autoimmune responses. This explains why some anti-inflammatory diets and supplements show promise. Particularly intriguing is research into the trigeminal nerve's role as both inflammation sensor and amplifier, potentially creating feedback loops that prolong attacks.
Blood Flow Mysteries
Contrary to past beliefs, vascular changes appear more as symptoms than causes. New models suggest blood vessel fluctuations represent the brain's failed attempts to rebalance oxygen and nutrients during neurological dysfunction. This paradigm shift influences drug development, with less emphasis on vasoconstriction and more on stabilizing neural activity.
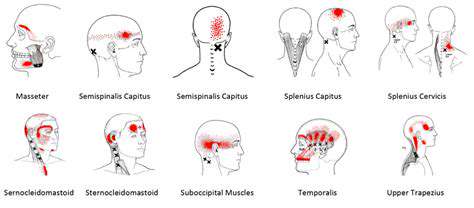
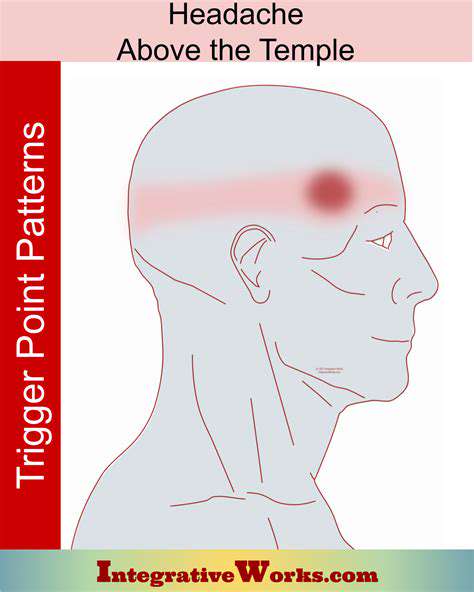
The Trigeminal Nerve's Double Life
This cranial nerve serves as the body's alarm system for head pain, but migraine transforms it into an overzealous security guard. Researchers study how normally separate pain pathways become cross-wired during attacks, creating the phenomenon where light, sound, and movement all intensify discomfort. Novel treatments aim to retrain these neural pathways using combined pharmacological and behavioral approaches.
Gut-Brain Conversations
The emerging gut microbiome research reveals surprising connections between digestive health and migraine frequency. Certain gut bacteria produce neurotransmitters or inflammatory molecules that may directly influence headache thresholds. This explains why some patients report improvement with probiotics or dietary changes, opening new prevention avenues beyond traditional neurology.
Mind-Body Approaches Gain Credibility
Once dismissed as soft science, biofeedback and mindfulness now boast clinical trial results rivaling medications for some patients. The recognition that stress hormones directly affect pain pathways has legitimized these approaches. Modern migraine clinics increasingly combine pharmaceutical interventions with cognitive behavioral therapy, creating comprehensive treatment plans addressing both biology and psychology.