HTML
Styling
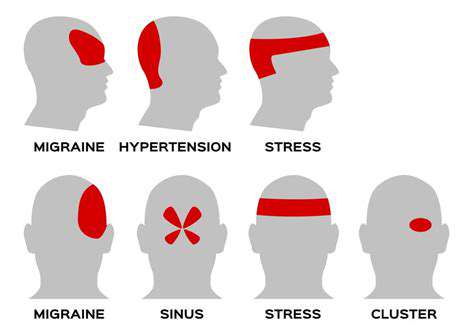
Neurology
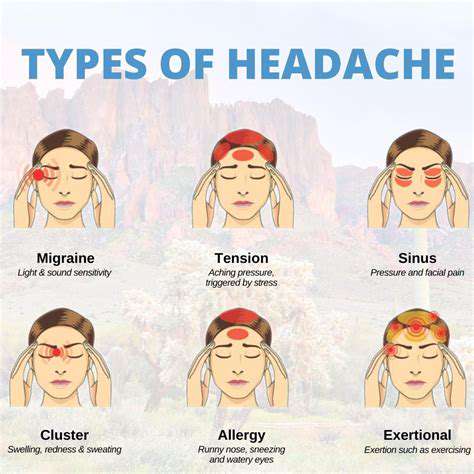
Migraine
CSS
Como o estresse crônico muda fisicamente o cérebro em pessoas com enxaqueca
A Nature Interligada de Estresse e Enxaqueca
Compreendendo a Ligação Estresse-Enxaqueca
O estresse crônico, um fator onipresente e muitas vezes subestimado na vida moderna, pode exercer uma profunda influência em nosso bem-estar físico, impactando diversos sistemas corporais. Uma consequência significativa do estresse crônico é a sua
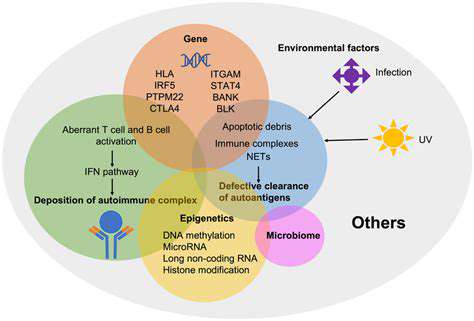
Desequilíbrios Neuroquímicos e Enxaqueca
Desregulação de Neurotransmissores
Desequilíbrios neuroquímicos, particularmente nos neurotransmissores do cérebro,
Read more about Como o estresse crônico muda fisicamente o cérebro em pessoas com enxaqueca
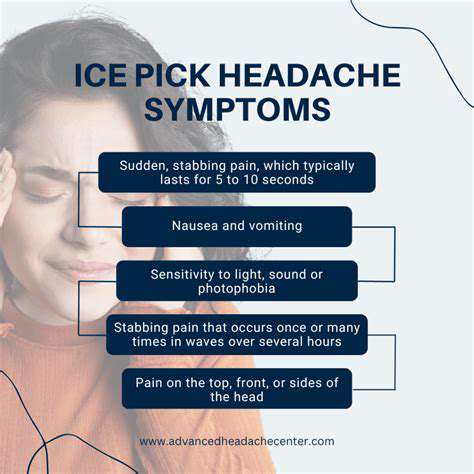
Cefaleias em Picadas de Gelo: Compreendendo a Dor Aguda e Perfurante
May 02, 2025
Melhorando a Higiene do Sono: Dicas para um Descanso Melhor e Menos Cefaleias
May 07, 2025
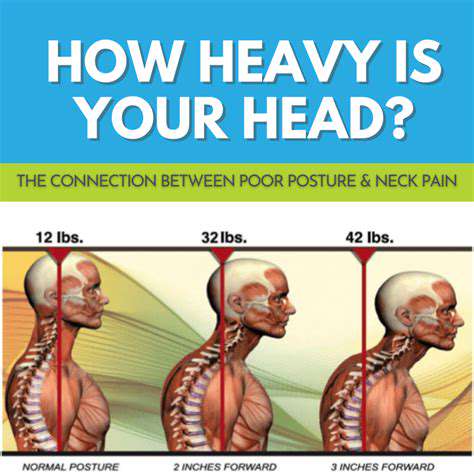
A Conexão Entre Distensão Cervical e Cefaleias de Tensão
May 19, 2025
Os descongestionantes podem ajudar ou prejudicar as dores de cabeça relacionadas aos seios da face?
May 31, 2025
Gerenciando Migrañas em um Trabalho de Alto Estresse
May 31, 2025
Ajustes Quiropráticos Podem Desencadear Enxaquecas?
Jun 25, 2025
Álcool e Enxaquecas: Compreendendo o Efeito Desencadenante
Jun 26, 2025
Cefaleias Exertionais: Quando o Exercício Desencadena a Dor
Jul 01, 2025
Como aprender seus gatilhos fortalece as escolhas diárias
Jul 03, 2025
Compreendendo como diferentes bebidas alcoólicas desencadeiam enxaquecas
Jul 05, 2025
A Base Neurológica da Migraine: Uma Mergulhada Profunda
Jul 11, 2025
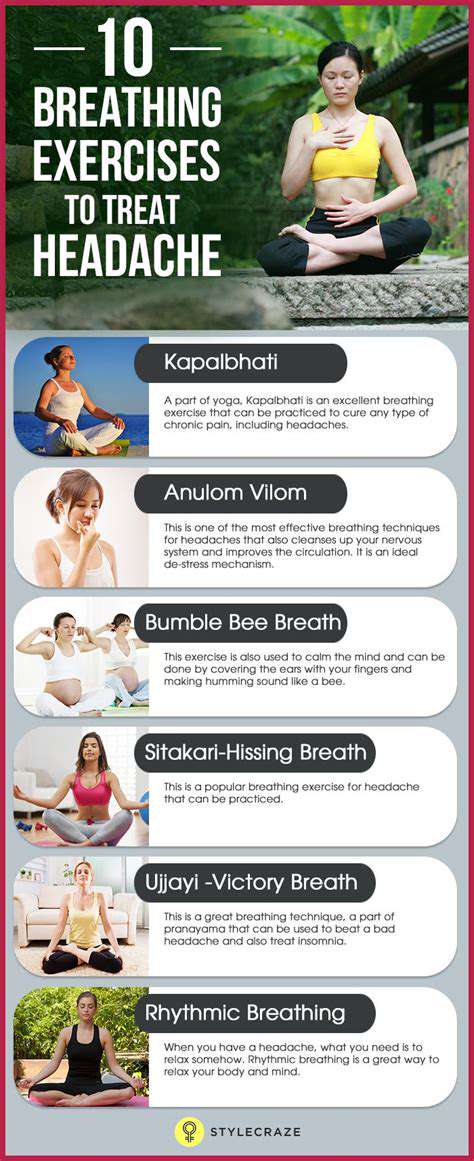
Práticas de Movimento Consciente para Sofredores de Cefaleia
Jul 12, 2025