HTML
Styling
Neurology
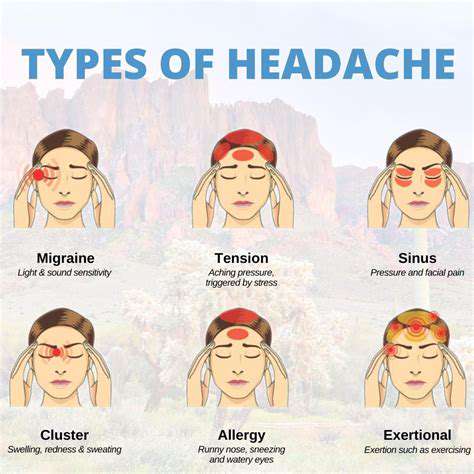
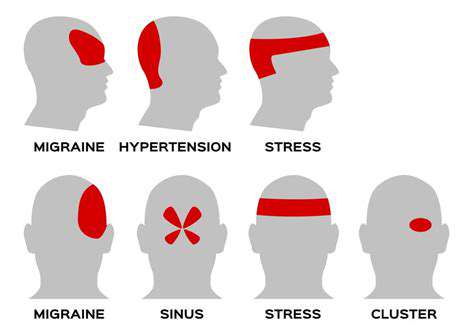
Migraine
CSS
慢性ストレスが片頭痛患者脳に及ぼす物理的な変化
ストレスと片頭痛の複雑な関係
ストレスと片頭痛の関係性について
現代社会において蔓延し、しばしば軽視される慢性的なストレスは、私たちの身体的健康に大きな影響を与え、様々な身体システムに影響を及ぼします。その深刻な結果の一つとして、長引く
神経化学的バランスの乱れと片頭痛
神経伝達物質の調節不全
神経化学的バランスの乱れ、特に脳内の神経伝達物質の調節不全は、片頭痛を引き起こす可能性のある重要な要因です。