Understanding Medication Overuse Headache (Rebound Headache)
The Initial Trigger
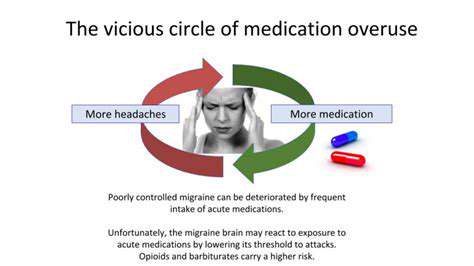
Many people start taking pain medication for completely legitimate reasons - perhaps for migraines, after an injury, or to manage chronic pain. The problem begins when occasional use turns into regular reliance, often without the person realizing how frequently they're reaching for the pills.
Without realizing it, people can start using medication not just to treat pain, but to prevent anticipated discomfort, which significantly increases overall consumption. This shift from treatment to prevention often marks the beginning of the overuse cycle.
Escalation and Dependence
As the body adapts to regular medication use, people often find they need higher doses to achieve the same pain relief. This happens because the brain becomes less responsive to the medication over time. At the same time, missing doses can lead to withdrawal symptoms that feel like headaches, creating the illusion that the medication is still needed for the original problem.
Perceived Ineffectiveness of Other Solutions
When medication seems to provide the most immediate relief, people naturally start doubting other approaches. They might try relaxation techniques or cold compresses but abandon them quickly if they don't work as fast as pills. This creates a mindset where medication appears to be the only effective solution, even though it's actually contributing to the problem.
Impact on Well-being
The consequences extend far beyond physical symptoms. Constant headaches and medication use can strain relationships, reduce work performance, and limit participation in enjoyable activities. Many people report feeling frustrated and hopeless as they struggle to break the cycle.
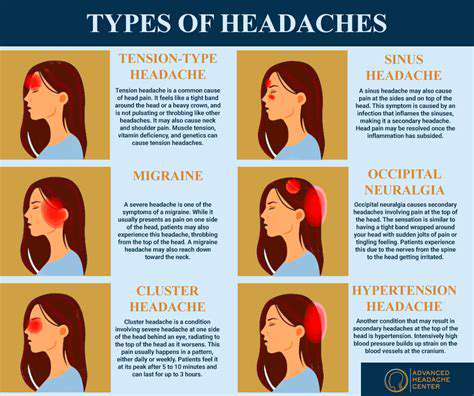
Perhaps most concerning is how medication overuse can hide underlying health issues that might need different treatment. For example, frequent headaches could signal sleep disorders, vision problems, or other conditions that require specific attention rather than just pain relief.
Seeking Relief from Side Effects
Ironically, the medications meant to help can create new problems. Some pain relievers cause stomach irritation, while others might lead to drowsiness or difficulty concentrating. People then sometimes take additional medications to manage these side effects, creating a complicated web of drug interactions.
Social and Economic Impacts
The ripple effects are substantial. Missed work days, medical expenses, and reduced productivity create financial strain. Socially, people may withdraw from activities they enjoy or become irritable with loved ones due to constant discomfort. The cumulative effect can significantly diminish quality of life.
Seeking Professional Help
Breaking free from this cycle almost always requires professional guidance. Doctors can help create a structured plan that addresses both the medication reduction and the original headache cause. This might involve alternative treatments, lifestyle changes, and sometimes therapy to address any psychological aspects of pain management.
Common Pain Relievers that Trigger Medication Overuse Headaches

Over-the-Counter Pain Relievers
Drugstore pain medications are convenient and effective for occasional use, but their easy availability makes them particularly likely candidates for overuse. Many people don't realize that taking these medications more than a couple of days a week can start the overuse cycle. They come in various forms - pills, liquids, even topical creams - but all carry this risk if used too frequently.
While generally safe when used occasionally, these medications become problematic with regular use. Reading labels carefully and tracking how often you take them can help prevent accidental overuse.
Acetaminophen
This popular pain and fever reducer works differently than anti-inflammatory drugs, making it suitable for people who can't take NSAIDs. However, its hidden danger lies in liver damage potential, especially when combined with alcohol or taken in doses exceeding recommendations. Many cold medicines and prescription painkillers also contain acetaminophen, creating risk of accidental overdose.
Despite these risks, acetaminophen remains a good option when used responsibly. The key is strict adherence to dosage guidelines and avoiding combination products unless specifically recommended by a doctor.
Ibuprofen
As an NSAID, ibuprofen reduces inflammation along with pain, making it effective for conditions like arthritis or sports injuries. Its anti-inflammatory properties make it popular, but these same properties increase risk of stomach irritation and other digestive issues with prolonged use.
Taking ibuprofen with food helps protect the stomach lining, and using the lowest effective dose for the shortest necessary time reduces risks. People with kidney issues or certain other health conditions should consult a doctor before regular use.
Naproxen
Similar to ibuprofen but longer-lasting, naproxen provides extended relief that can be helpful for chronic conditions. This extended action means fewer doses are needed throughout the day, but it also means the drug remains in the system longer, increasing potential for cumulative effects.
Other Pain Relievers
The pain relief aisle contains numerous options, from aspirin to combination products. Some contain caffeine, which can both help with headaches and contribute to rebound effects. Others combine different pain relievers, which might seem more effective but actually increase risks without providing clear benefits.
Interactions and Precautions
Mixing pain relievers or combining them with other medications requires caution. Some combinations can cause dangerous interactions, while others might simply cancel each other out. For example, taking multiple NSAIDs together increases side effect risks without improving pain relief.
Always inform healthcare providers about all medications and supplements you're taking, including occasional pain relievers. Pharmacists can also provide valuable advice about potential interactions and safer alternatives.