HTML
CSS
Pain Management
Musculoskeletal Disorders
Myofascial Pain
Dry Needling
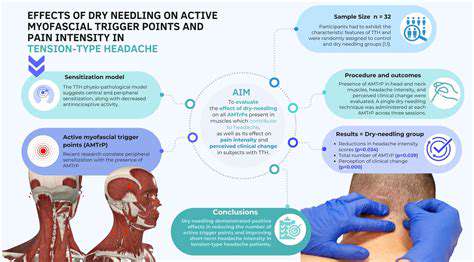
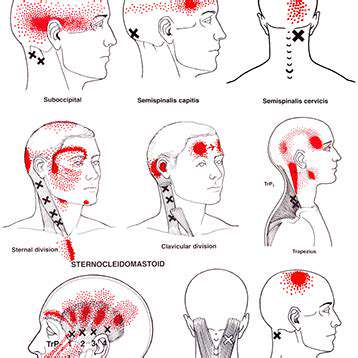
筋膜痛と頭痛に対するドライニードリングの探求
筋膜性疼痛症候群と頭痛の関係を探る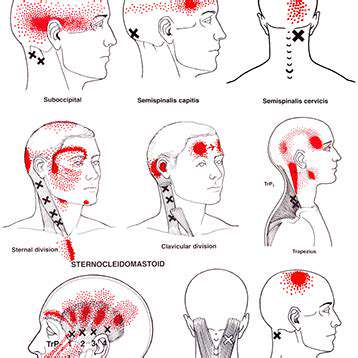
Read more about 筋膜痛と頭痛に対するドライニードリングの探求
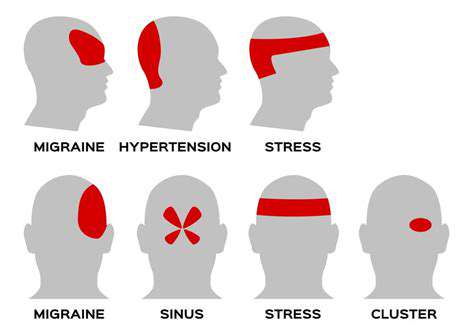
群発頭痛を理解する:原因、症状、治療法メタ説明:群発頭痛の複雑さを探求し、その原因や症状から効果的な治療法までを学びます。この重篤な頭痛状態を専門家の洞察と対処戦略を用いて管理する方法を知りましょう。内容概要:群発頭痛は、周期的に現れる強烈で無力にさせる頭痛で、しばしば頭の片側に激しい痛みが生じます。鼻づまりや涙が出るなどの特有の症状を理解することは、効果的な管理に不可欠です。これらの頭痛は遺伝的要因、生体リズム、環境要因によるもので、日常生活に大きな影響を与えることがあります。治療は、即効性を重視した酸素療法やトリプタンを用いる急性の手段と、予防薬を伴うことが多いです。ライフスタイルの変更や個々のトリガーに対する認識は管理戦略を向上させる可能性があり、代替療法やサポートグループも追加の支援を提供します。群発頭痛の課題を乗り越え、情報に基づく戦略と専門家の指導を通じて生活の質を向上させる方法を見つけましょう。
Oct 11, 2024
原因、影響、そして和らげる戦略頭痛と首の痛みは、日常生活や生産性に大きな影響を及ぼす一般的な問題です。この包括的なガイドでは、悪い姿勢や筋肉の緊張、ストレス、基礎的な健康状態に至るまで、さまざまな原因を探ります。痛みが続く場合は、専門の医療アドバイスを求めることの重要性に加え、症状を和らげることができる効果的な家庭療法やライフスタイルの変更についても説明します。主なテーマは以下の通りです:- 日常生活への影響:頭痛と首の痛みは、日常の活動を妨げ、精神的健康に連鎖的な影響を与える可能性があります。- 一般的な原因:筋肉の緊張、ストレス、怪我など、痛みの原因となる要因について学びます。- 医療相談:専門家の助けを求めるべき時期と、個別の治療の利点を理解します。- 家庭療法:人間工学的調整、エクササイズ、マインドフルネスの実践といった効果的な戦略を探ります。- 代替療法:鍼治療、マッサージ療法、カイロプラクティックがどのように従来の治療を補完できるかを発見します。頭痛と首の痛みに悩む人にとって、これらの要素を理解することは、効果的な痛みの管理と全体的な健康にとって非常に重要です。ホリスティックなアプローチを優先することで、生活の質は大きく向上する可能性があります。
Oct 15, 2024
咳嗽中の筋肉の緊張を理解する:原因、症状、緩和策メタ説明:咳嗽による筋肉の緊張の原因、一般的な症状、効果的な緩和策を発見してください。呼吸器の健康を改善するために筋肉の緊張を予防し、管理する方法を学びましょう。---咳嗽中に筋肉が緊張する原因は何ですか?咳嗽は気道をクリアするための自然な反射ですが、特に胸部や腹部で筋肉の緊張を引き起こすことがあります。この記事では、咳嗽中の筋肉の緊張のメカニズム、一般的な悪化要因、全体的な筋肉の健康の重要な役割を探ります。咳嗽による筋肉緊張の症状局所的な痛み、圧迫感、腫れなどの症状を認識する方法を学びましょう。これらの兆候を理解することは、不快感の管理や慢性的な問題の予防に重要です。予防策と緩和策咳嗽による筋肉の緊張を予防するための実用的なヒントを探求し、呼吸の健康、水分補給、正しい呼吸法を維持することを含めます。温熱療法や冷却療法、穏やかなストレッチなどの効果的な緩和法を発見し、いつ医療相談を受けるべきかを判断しましょう。自分の健康を強化する咳嗽と筋肉の緊張の関係を理解することで、健康管理のための積極的な手段を講じましょう。医療専門家に相談し、筋肉を強化するための運動に取り組んで、より良いレジリエンスを手に入れましょう。咳嗽による筋肉の緊張を予防し、管理するためのさらなる洞察を得るために、私たちの完全ガイドを訪問してください!
Dec 31, 2024