Exploring Dry Needling for Myofascial Pain and Headaches
Understanding Myofascial Pain Syndrome (MPS)
Myofascial pain syndrome represents a persistent pain disorder where individuals experience localized discomfort and sensitivity in particular body regions, primarily due to trigger points. These muscular knots can create referred pain patterns, causing discomfort in seemingly unrelated areas. Successful management hinges on accurate trigger point identification and treatment, as these factors directly influence long-term symptom relief. Patients often report substantial interference with routine activities and quality of life.
The nature of MPS pain typically manifests as a deep, persistent ache with fluctuating intensity. Its ability to mimic other musculoskeletal conditions frequently complicates diagnosis. While the exact etiology remains unclear, clinical observations point to multiple contributing elements including repetitive strain, traumatic injuries, psychological stress, and postural imbalances. A comprehensive evaluation by a qualified specialist, incorporating both physical assessment and diagnostic imaging when necessary, remains essential for differential diagnosis. Timely therapeutic intervention often yields better prognosis and prevents chronic pain development.
The Headache Connection in MPS
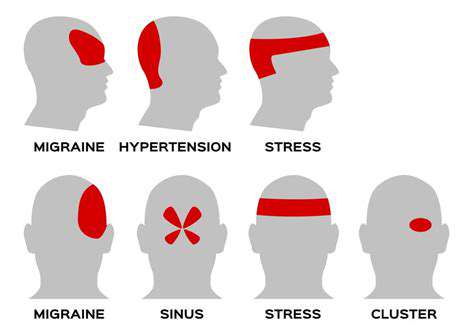
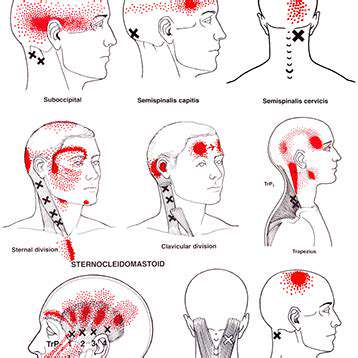
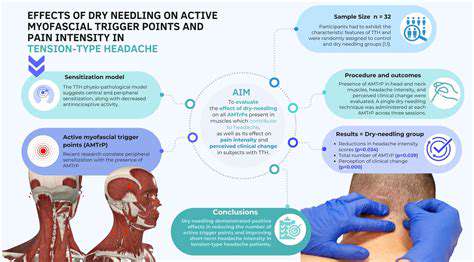
Many individuals with myofascial dysfunction experience cephalalgia originating from activated trigger points in cervical and cranial musculature. These hyperirritable zones can generate various headache phenotypes, including tension-type patterns and migraine-like symptoms. The resultant pain spectrum ranges from dull pressure to sharp, debilitating sensations that impair normal functioning. Precise mapping of causative trigger points forms the foundation of effective headache management in these cases.
Tension-type cephalalgia associated with myofascial pathology often presents as persistent band-like pressure around the cranium, frequently accompanied by cervical stiffness. Common exacerbating factors include emotional stress, prolonged static postures, and routine physical activities. Successful management requires focused attention on muscular tension reduction and specific trigger point inactivation. The pain frequently exhibits radiation patterns extending from occipital to frontal regions.
While the migraine-MPS relationship requires further investigation, emerging evidence suggests potential interactions between these conditions. The complex pathophysiology warrants consideration of myofascial components when evaluating refractory headache cases. Comprehensive treatment planning should incorporate potential myofascial contributions to cephalalgic symptoms.
Dry Needling: A Therapeutic Approach for Myofascial Pain and Cephalalgia
Mechanisms of Dry Needling in Myofascial Pathology
This intervention utilizes filamentous needles to precisely target dysfunctional myofascial tissues, including muscular, tendinous, and fascial structures. Therapeutic needle insertion creates localized mechanical and biochemical changes that facilitate pain modulation and functional restoration. Clinical observations demonstrate particular efficacy in chronic myofascial conditions characterized by persistent trigger point activity.
The hallmark features of myofascial pathology - localized tenderness, referred pain patterns, and restricted mobility - respond favorably to precise needling interventions. The technique's therapeutic value stems from its capacity to mechanically disrupt pathological trigger point architecture while stimulating endogenous pain control mechanisms.
Pathophysiology of Trigger Points
Myofascial trigger points represent hyperirritable foci within taut muscle bands, developing secondary to various mechanical and metabolic stressors. These pathological zones generate characteristic pain referral patterns that complicate clinical assessment. Effective management requires comprehensive understanding of trigger point physiology and biomechanical relationships.
Active trigger points create significant functional impairment through multiple mechanisms including motor inhibition, altered movement patterns, and sustained nociceptive input. These changes frequently lead to progressive physical deconditioning if left unaddressed.
Fascial Contributions to Pain Syndromes
The fascial network provides essential structural and functional integration throughout the musculoskeletal system. Pathological changes in fascial elasticity and hydration status contribute substantially to pain generation and movement dysfunction. These alterations frequently coexist with myofascial trigger point pathology.
Contemporary treatment approaches recognize the importance of addressing fascial restrictions concurrently with muscular dysfunction. This integrated strategy often yields more durable therapeutic outcomes compared to isolated interventions.
Clinical Considerations for Dry Needling
When administered by properly credentialed clinicians, dry needling demonstrates an excellent safety profile. However, appropriate patient selection and procedural technique remain paramount for risk minimization. Comprehensive pretreatment evaluation should identify potential contraindications and establish clear treatment objectives.
Practitioners must maintain rigorous infection control standards and possess thorough knowledge of regional anatomy to prevent adverse events. Patient education regarding expected post-treatment responses enhances compliance and satisfaction.
Importance of Clinical Expertise
Optimal outcomes require practitioners with specialized training in both needling techniques and comprehensive musculoskeletal assessment. Inadequate preparation may compromise treatment efficacy or patient safety. Clinicians should demonstrate proficiency in differential diagnosis and treatment planning.
Individualized treatment protocols based on thorough clinical evaluation typically yield superior results compared to standardized approaches. This patient-centered methodology accounts for unique anatomical variations and pain patterns.
Multidimensional Therapeutic Benefits
Beyond analgesia, dry needling facilitates functional improvements including enhanced joint mobility and muscular coordination. By addressing the underlying pathophysiology of myofascial dysfunction, this modality supports comprehensive rehabilitation strategies. These effects prove particularly valuable in chronic pain populations.
The intervention's neuromodulatory effects often produce secondary benefits such as postural optimization and movement efficiency. When integrated with other therapeutic modalities, dry needling enhances overall treatment effectiveness.
Fundamentally, mindful parenting cultivates enhanced situational awareness encompassing both child behaviors and parental emotional responses. This intentional approach facilitates recognition of how parental reactions shape child development and emotional regulation. Developing this awareness creates opportunities for more authentic and nurturing relationships that foster secure attachment. The process involves identifying personal emotional triggers and implementing constructive response patterns.