HTML
Styling
Neurological Conditions
Medical Technology
Neurostimulation
Pain Management
ClinicalTrials
TreatmentEvaluation
偏頭痛治療のための神経調節デバイス(例:Cefaly、Nerivio)
深い探求
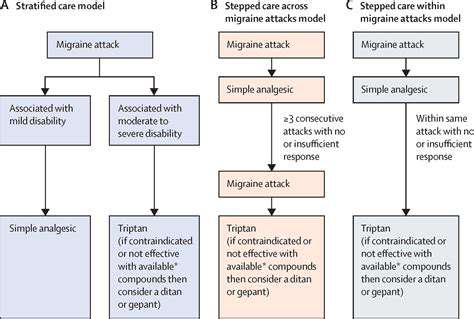
神経調節デバイスは、電気刺激を一般的な方法として用いています。この技術は、特定の神経経路に制御された電気的インパルスを供給するものです。これらのインパルスは、しばしば片頭痛発作の根底にある異常な電気活動に干渉することができます。正確な位置と強度は、
Cefaly:経皮的デバイスの深い探求
Cefalyの作用機序
Cefaly、経皮的神経刺激デバイスは、特定の頭蓋骨部位に正確に調整された電気パルスを供給するという原理で動作します。
神経調節デバイスの有効性と安全性の評価

有効性の評価
慢性疼痛緩和のための効果的な疼痛管理戦略を評価する
Read more about 偏頭痛治療のための神経調節デバイス(例:Cefaly、Nerivio)
効果的な治療のための痛みの認識を理解するメタディスクリプション:治療における痛みの認識の重要性を発見し、重要な痛み評価ツール、管理戦略に対する痛みの頻度の影響、急性痛と慢性痛の違いについて探究します。医療専門家とのコラボレーションが痛み管理を強化し、生活の質を向上させる方法を学びます。---導入:痛みの認識は効果的な治療計画に不可欠です。数値評価尺度(NRS)や視覚的アナログ尺度(VAS)などの評価ツールを利用することで、医療専門家は患者の痛みのレベルを理解し、痛み管理のための個別化された戦略を保証します。主なトピック:- 痛み評価ツールの役割:痛みを効果的に伝え、個別化された治療計画を立てる。- 痛みの頻度の影響:慢性痛と間欠的痛が治療の決定にどのように影響するかを学ぶ。- 痛みの分類:急性痛を短期応答、慢性痛を長期的な課題として理解。- 痛みの強度の評価:強度が生活の質に与える影響と個別化された評価戦略の必要性を発見。- 協力的アプローチ:医療専門家と協力して多職種連携のアプローチで痛み管理に取り組む。結論:痛みの認識と管理戦略についての知識を持つことで、自分自身を強化します。主導的になり、医療専門家と関わることで、個人は痛みの管理成果と全体的な生活の質を向上させることができます。
Oct 14, 2024
左側の鋭い痛みの一般的な原因左側の鋭い痛みの一般的な原因には、筋骨格系の問題、消化器の障害、心臓に関する懸念が含まれます。この包括的なガイドでは、左側の痛みに関連する症状と潜在的な診断について説明し、早期発見と治療の重要性を強調します。筋肉の緊張や靭帯の捻挫による筋骨格系の痛み、胃炎や憩室炎などの消化器系の問題、狭心症や心臓発作などの深刻な心臓の状態を学びましょう。医療の助けを求めるべき時期やさまざまな治療オプションについて理解することが重要です。健康に関する情報を把握し、ウェルネスに向けて積極的なステップを踏み出しましょう。キーワード:左側の鋭い痛み、筋骨格系の痛み、消化器疾患、心臓に関する懸念、痛みの診断、治療オプション、医療の助けを求める
Oct 28, 2024
頭痛を理解する
頭痛に関する包括的なガイドへようこそ。この一般的な病気の複雑さを掘り下げていきます。偏頭痛、緊張型頭痛、群発頭痛などの種類を含む一次性と二次性頭痛の違いを発見しましょう。ストレスや睡眠不足、食事の影響など、これらの頭痛を悪化させる可能性のある一般的なトリガーを探ります。市販薬からライフスタイルの調整、非薬物療法に至るまで、特定の頭痛タイプに合わせた効果的な治療オプションを学びます。私たちのリソースはまた、医学的援助を求めるタイミングや、あまり一般的でない頭痛に関する洞察を強調し、あなたが症状をうまく管理できるようにします。最新の研究や個別化されたアプローチを通じて情報を得て、生活の質を向上させ、頭痛のトリガーを特定し、あなたに合った緩和戦略を見つけましょう。
Oct 31, 2024
左側頭部の脈動痛を理解し、症状、緊張型頭痛や偏頭痛などの一般的な原因、効果的な治療オプションを探ります。この包括的なガイドは、脈動痛の特徴、拍動感や間欠性を含む特性、吐き気や光への敏感さなどの可能な伴随症状を深く掘り下げます。生活習慣要因、環境トリガー、基礎疾患がこの不快感にどのように寄与するかを学びます。偏頭痛、群発頭痛、側頭動脈炎などの一般的な原因について知り、重症症状に対していつ医療機関に相談すべきかを理解します。このページでは、痛みを和らげるための薬剤選択、食事への配慮、生活習慣の変更を含むさまざまな管理戦略も紹介されています。脈動痛を効果的に管理し、全体的な健康を改善するための知識を身につけましょう。
Nov 09, 2024
後頭部の痛みの一般的な原因メタ説明:筋肉の緊張、偏頭痛、頚椎の問題、そして副鼻腔感染など、後頭部の痛みの一般的な原因を発見しましょう。症状を管理する方法や、慢性的な不快感に対して医療援助を求めるべき時期を学んでください。タイトル:後頭部の痛みの理解内容概要:この包括的なガイドでは、後頭部の痛みの最も一般的な原因を探り、筋肉の緊張、偏頭痛、緊張性頭痛、頚椎の問題、そして副鼻腔の問題に関する洞察を提供します。症状を特定することに加えて、この記事では不快感を和らげ、全体的な健康を改善するための治療オプションと自己管理戦略についても掘り下げます。主なセクション:- 筋肉の緊張と緊張:姿勢とストレスが首や肩の痛みにどのように寄与するかを発見します。- 偏頭痛と緊張性頭痛:症状、引き金、および効果的な管理技術について学びます。- 頚椎の問題:脊柱の健康が頭痛や首の痛みに与える影響を理解します。- 副鼻腔の問題と感染:副鼻腔の不快感と頭痛の関連を特定し、緩和オプションを探ります。- その他の要因:脱水、環境の引き金、ストレスも頭痛の発生と重症度において重要な役割を果たします。- 医療援助の要請:持続的または深刻な症状について医療専門家に相談するタイミングに関するガイダンス。行動の呼びかけ:後頭部に慢性的な痛みを感じている方や、症状管理に関するカスタマイズされたアドバイスが必要な方は、個別の治療計画のために医療提供者に相談してください。
Dec 10, 2024