HTML
Styling
Neurological Conditions
Medical Technology
Neurostimulation
Pain Management
ClinicalTrials
TreatmentEvaluation
用於偏頭痛治療的神經調控裝置(例如,Cefaly、Nerivio)
深入探討
電刺激是神經調節裝置常用的方法。此技術涉及將受控的電脈衝傳送至特定的神經通路。這些脈衝可以干擾通常存在於偏頭痛發作的異常電活動。精確的部位以及
Cefaly:深入探討經皮神經刺激裝置
Read more about 用於偏頭痛治療的神經調控裝置(例如,Cefaly、Nerivio)
理解疼痛識別以實現有效治療元描述:發現疼痛識別在治療中的重要性。探索基本的疼痛評估工具,疼痛頻率對管理策略的影響,以及急性疼痛與慢性疼痛之間的差異。了解如何與醫療專業人員合作以增強疼痛管理,並改善生活品質。---引言:疼痛識別對有效治療計劃至關重要。利用數字評分量表(NRS)和視覺模擬量表(VAS)等評估工具,幫助醫療專業人員了解病患的疼痛水準,確保量身定制的疼痛管理策略。重點話題:- 疼痛評估工具的作用:有效溝通疼痛並制定個性化治療計劃。- 疼痛頻率的影響:了解慢性疼痛與間歇性疼痛如何影響治療決策。- 疼痛分類:理解急性疼痛為短期反應,慢性疼痛為長期挑戰。- 評估疼痛強度:發現強度如何影響生活品質以及個性化評估策略的必要性。- 協作方法:與醫療專業人員交流,共同採用多學科的方法進行疼痛管理。結論:通過了解疼痛識別與管理策略,賦予自己權力。通過保持主動並與醫療專業人員互動,個人可以改善疼痛管理結果和整體生活品質。
Oct 14, 2024
左側劇烈疼痛的常見原因探索左側劇烈疼痛的常見原因,包括肌肉骨骼問題、胃腸疾病和心臟問題。本綜合指南討論與左側疼痛相關的症狀和潛在診斷,強調早期發現和治療的重要性。了解由肌肉拉傷和韌帶扭傷引起的肌肉骨骼疼痛,胃炎和憩室炎等胃腸問題,以及如心絞痛和心臟病發作等嚴重的心臟病情況。了解何時尋求醫療幫助和可用的各種治療選項。保持健康資訊的更新,並採取主動措施走向健康。關鍵字:左側劇烈疼痛,肌肉骨骼疼痛,胃腸疾病,心臟問題,疼痛診斷,治療選擇,尋求醫療幫助
Oct 28, 2024
了解頭痛
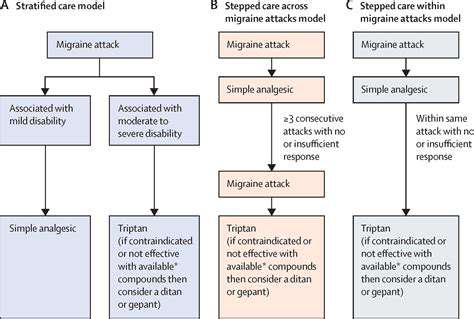
歡迎來到我們關於頭痛的綜合指南,我們將深入探討這一常見疾病的複雜性。了解原發性和繼發性頭痛之間的主要差異,包括偏頭痛、緊張型頭痛和叢集性頭痛等類型。探索可能加劇這些頭痛的常見誘因,從壓力和睡眠不足到飲食影響。了解針對特定頭痛類型的有效治療方案,從非處方藥物到生活方式調整和非藥物治療。我們的資源還強調何時尋求醫療幫助,並提供對較少見頭痛的見解,確保您能夠有效地管理症狀。保持了解最新的研究和個性化的方法,以幫助改善您的生活品質,使您能夠識別頭痛誘因並發現適合您的緩解策略。
Oct 31, 2024
理解左側頭部的脈動疼痛,探索其症狀、常見原因(如緊張性頭痛和偏頭痛)以及有效的治療選擇。本綜合指南深入探討脈動疼痛的特徵,包括其搏動感和間歇性,還包括可能伴隨的症狀,如噁心和對光敏感。了解生活方式因素、環境誘因和潛在的醫療條件如何加劇這種不適。了解偏頭痛、叢集性頭痛和顳動脈炎等常見原因,並了解何時因嚴重症狀尋求醫療幫助。頁面還強調了各種管理策略,包括藥物選擇、飲食考慮和生活方式的調整,以減輕疼痛。用知識為自己賦能,有效管理脈動疼痛,提高整體健康水平。
Nov 09, 2024
後腦痛的常見原因元描述:了解導致後腦痛的常見原因,包括肌肉拉傷、偏頭痛、頸椎問題和鼻竇感染。學習如何管理症狀,以及何時尋求醫療幫助以應對慢性不適。標題:理解後腦痛內容概述:本綜合指南探討了後腦痛的最常見原因,提供有關肌肉拉傷、偏頭痛、緊張性頭痛、頸椎問題和鼻竇問題的見解。文章除識別症狀外,還探討了緩解不適和改善整體健康的治療方案和自我護理策略。主要部分:- 肌肉拉傷和緊張:發現姿勢和壓力如何導致頸部和肩膀疼痛。- 偏頭痛和緊張性頭痛:了解症狀、觸發因素和有效的管理技巧。- 頸椎問題:了解脊柱健康對頭痛和頸部疼痛的影響。- 鼻竇問題和感染:識別鼻竇不適與頭痛之間的聯繫,並探索緩解選項。- 其他因素:脫水、環境觸發因素和壓力也在頭痛的發生和嚴重性中起關鍵作用。- 尋求醫療幫助:關於何時諮詢醫療專業人員以應對持續或嚴重症狀的指南。行動呼籲:如果你正經歷後腦的慢性疼痛或需要針對症狀管理提供量身定制的建議,請諮詢醫療提供者以獲取個性化的治療方案。
Dec 10, 2024