HTML
Styling
Neurological Conditions
Medical Technology
Neurostimulation
Pain Management
ClinicalTrials
TreatmentEvaluation
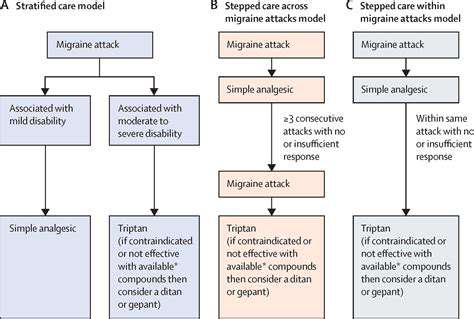
用于偏头痛治疗的神经调控设备(例如,Cefaly、Nerivio)
深入探讨
电刺激是神经调控设备常用的方法。这种技术涉及向特定神经通路传递受控的电脉冲。这些脉冲可以干扰通常存在于偏头痛发作之下的异常电活动。精确的定位和内
Cefaly:深入探讨经皮设备
Read more about 用于偏头痛治疗的神经调控设备(例如,Cefaly、Nerivio)
理解疼痛识别以实现有效治疗元描述:发现疼痛识别在治疗中的重要性。探索基本的疼痛评估工具,疼痛频率对管理策略的影响,以及急性疼痛与慢性疼痛之间的差异。了解如何与医疗专业人员合作以增强疼痛管理,并改善生活质量。---引言:疼痛识别对有效治疗计划至关重要。利用数字评分量表(NRS)和视觉模拟量表(VAS)等评估工具,帮助医疗专业人员了解患者的疼痛水平,确保量身定制的疼痛管理策略。重点话题:- 疼痛评估工具的作用:有效沟通疼痛并制定个性化治疗计划。- 疼痛频率的影响:了解慢性疼痛与间歇性疼痛如何影响治疗决策。- 疼痛分类:理解急性疼痛为短期反应,慢性疼痛为长期挑战。- 评估疼痛强度:发现强度如何影响生活质量以及个性化评估策略的必要性。- 协作方法:与医疗专业人员交流,共同采用多学科的方法进行疼痛管理。结论:通过了解疼痛识别与管理策略,赋予自己权力。通过保持主动并与医疗专业人员互动,个人可以改善疼痛管理结果和整体生活质量。
Oct 14, 2024
左侧剧烈疼痛的常见原因探索左侧剧烈疼痛的常见原因,包括肌肉骨骼问题、胃肠疾病和心脏问题。本综合指南讨论与左侧疼痛相关的症状和潜在诊断,强调早期发现和治疗的重要性。了解由肌肉拉伤和韧带扭伤引起的肌肉骨骼疼痛,胃炎和憩室炎等胃肠问题,以及如心绞痛和心脏病发作等严重的心脏病情况。了解何时寻求医疗帮助和可用的各种治疗选项。保持健康信息的更新,并采取主动措施走向健康。关键词:左侧剧烈疼痛,肌肉骨骼疼痛,胃肠疾病,心脏问题,疼痛诊断,治疗选择,寻求医疗帮助
Oct 28, 2024
了解头痛
欢迎来到我们有关头痛的综合指南,我们将深入探讨这一常见疾病的复杂性。了解原发性和继发性头痛之间的主要区别,包括偏头痛、紧张型头痛和丛集性头痛等类型。探索可能加剧这些头痛的常见诱因,从压力和睡眠不足到饮食影响。了解针对特定头痛类型的有效治疗方案,从非处方药物到生活方式调整和非药物治疗。我们的资源还强调何时寻求医疗帮助,并提供对较少见头痛的见解,确保您能够有效地管理症状。保持了解最新的研究和个性化的方法,以帮助改善您的生活质量,使您能够识别头痛诱因并发现适合您的缓解策略。
Oct 31, 2024
理解左侧头部的跳动疼痛,探索其症状、常见原因(如紧张性头痛和偏头痛)以及有效的治疗选择。本综合指南深入探讨跳动疼痛的特征,包括其搏动感和间歇性,还包括可能伴随的症状,如恶心和对光敏感。了解生活方式因素、环境诱因和潜在的医疗条件如何加剧这种不适。了解偏头痛、丛集性头痛和颞动脉炎等常见原因,并了解何时因严重症状寻求医疗帮助。页面还强调了各种管理策略,包括药物选择、饮食考虑和生活方式的调整,以减轻疼痛。用知识为自己赋能,有效管理跳动疼痛,提高整体健康水平。
Nov 09, 2024
后脑疼痛的常见原因元描述:了解导致后脑疼痛的常见原因,包括肌肉拉伤、偏头痛、颈椎问题和窦道感染。学习如何管理症状,以及何时寻求医疗帮助以应对慢性不适。标题:理解后脑疼痛内容概述:本综合指南探讨了后脑疼痛的最常见原因,提供有关肌肉拉伤、偏头痛、紧张性头痛、颈椎问题和窦道问题的见解。文章除识别症状外,还探讨了缓解不适和改善整体健康的治疗方案和自我护理策略。主要部分:- 肌肉拉伤和紧张:发现姿势和压力如何导致颈部和肩膀疼痛。- 偏头痛和紧张性头痛:了解症状、触发因素和有效的管理技巧。- 颈椎问题:了解脊柱健康对头痛和颈部疼痛的影响。- 窦道问题和感染:识别窦道不适与头痛之间的联系,并探索缓解选项。- 其他因素:脱水、环境触发因素和压力也在头痛的发生和严重性中起关键作用。- 寻求医疗帮助:关于何时咨询医疗专业人员以应对持续或严重症状的指南。行动呼吁:如果你正经历后脑的慢性疼痛或需要针对症状管理提供量身定制的建议,请咨询医疗提供者以获取个性化的治疗方案。
Dec 10, 2024