Headaches
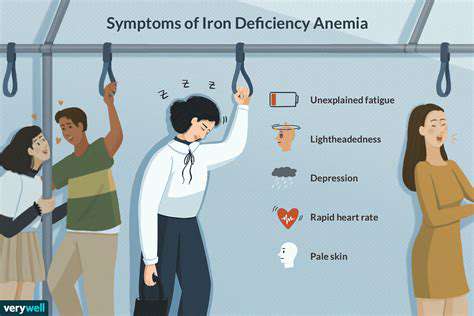
Medical Conditions
HTML
Styling
Sleep Disorders
Migraine Triggers
Hormonal Imbalance
Headache Triggers
CSS
Psychology
Wellbeing
두통 유발 10가지 흔한 편두통 유발 요인
두통의 원흉을 파악하기
편두통 유발 요인의 수수께끼 이해하기
편두통, 그 고통스러운 두통은 종종 예고 없이 찾아와 고통받는 사람들을 극심한 고통 속에 빠뜨립니다. 편두통의 정확한 원인은 아직 밝혀지지 않았지만,
2. 수면 패턴 변화: 깨진 리듬
Read more about 두통 유발 10가지 흔한 편두통 유발 요인
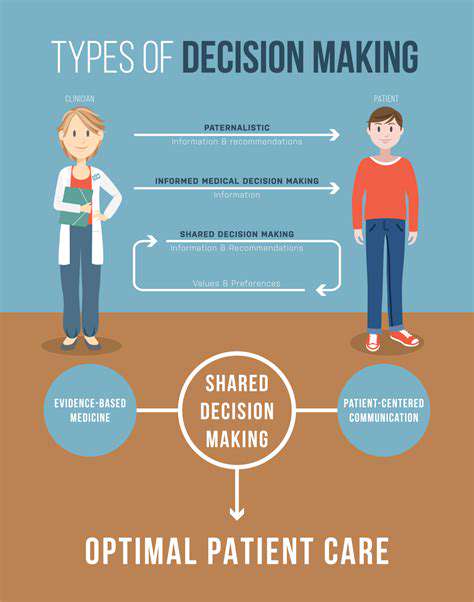
두피 통증의 일반적인 원인을 파악하고 효과적인 치료 옵션을 탐구하세요. 우리의 포괄적인 가이드는 편두통 및 긴장성 두통에서부터 건선과 신경 관련 통증 같은 두피 상태에 이르기까지 모든 것을 다룹니다. 증상 인식의 중요성, 기저 질환 관리, 불편을 완화하기 위한 약물 및 가정 요법 활용에 대해 알아보세요. 라이프스타일 변경을 통해 웰빙을 향상시키고 두피 건강을 위한 맞춤형 솔루션을 찾으세요. 오늘 지속적인 두피 통증에 대한 정보를 얻고 구제를 찾아보세요!
Nov 22, 2024
원인, 증상 및 치료머리 중간의 통증은 괴롭힐 수 있습니다. 이 포괄적인 가이드는 두통의 일반적인 원인을 파헤치고 증상과 유발 요인, 치료 옵션, 그리고 의료 도움을 요청해야 할 시기를 설명합니다.
Apr 10, 2025