Headaches
Medical Conditions
HTML
Styling
Sleep Disorders
Migraine Triggers
Hormonal Imbalance
Headache Triggers
CSS
Psychology
Wellbeing
10 najczęściej występujących czynników wywołujących migrenę, których należy unikać
Rozpoznawanie przyczyn migreny
View Blog>>
Zrozumienie zagadki czynników wywołujących migrenę
Migreny, te upośledzające bóle głowy, często uderzają bez ostrzeżenia, pozostawiając cierpiących w dręczącym bólu. Podczas gdy dokładna przyczyna migren pozostaje zagadką,
2. Zmiany w wzorcach snu: Zakłócony rytm
Zmiany w wzorcach snu i migreny
Zakłócenia snu, niezależnie od tego, czy wynikają z niedoboru snu, nieregularnych harmonogramów snu, czy zaburzeń snu, często wiążą się z atakami migreny. Mechanizmy Wahania poziomów estrogenu i progesteronu w cyklu menstruacyjnym stanowią istotny czynnik dla wielu kobiet doświadczających bólów głowy Przeciążenie zmysłów jest częstym
5. Wahania hormonalne: Miesięczny cykl bólów głowy
Zmiany hormonalne i czynniki wywołujące bóle głowy
9. Przeciążenie Zmysłów: Przeciążenie Zmysłów

Przeciążenie Zmysłów: Częsta Zdarzenie
Read more about 10 najczęściej występujących czynników wywołujących migrenę, których należy unikać
Odkryj powszechne przyczyny bólu skóry głowy i zbadaj skuteczne opcje leczenia. Nasz kompleksowy przewodnik obejmuje wszystko, od migren i bólów głowy spowodowanych stresem, po schorzenia skóry głowy, takie jak łuszczyca i ból związany z nerwami. Dowiedz się o znaczeniu rozpoznawania objawów, zarządzania schorzeniami podstawowymi i korzystania z leków oraz domowych środków zaradczych, aby złagodzić dyskomfort. Popraw swoje samopoczucie dzięki zmianom w stylu życia i poszukaj spersonalizowanych rozwiązań dla zdrowia skóry głowy. Zdobądź informacje i znajdź ulgę od uporczywego bólu skóry głowy już dziś!
Nov 22, 2024
Przyczyny, Objawy i LeczenieDoświadczanie bólu w środku głowy może być niepokojące. Ten kompleksowy przewodnik bada powszechne przyczyny bólu głowy, identyfikuje objawy i wyzwalacze, opcje leczenia oraz kiedy szukać pomocy medycznej.
Apr 10, 2025
Nowa, utrzymująca się codzienna migrena (NDPH): Co musisz wiedzieć
May 14, 2025
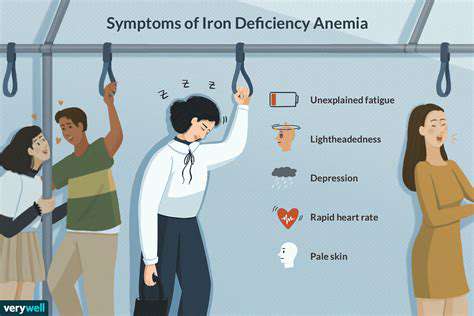
Niedokrwistość z niedoboru żelaza i bóle głowy: Co musisz wiedzieć
May 24, 2025
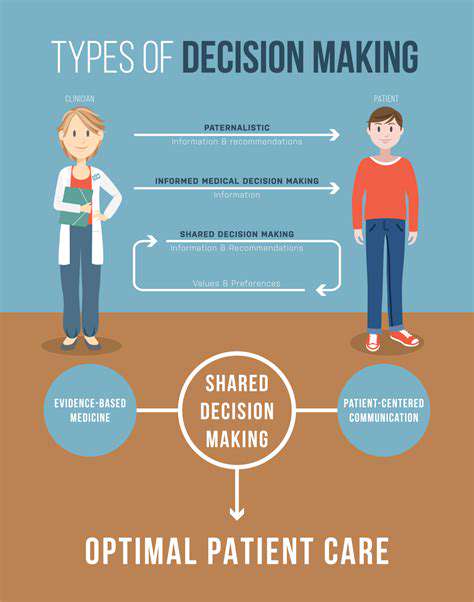
Rozmowa z lekarzem o planie leczenia migreny
May 31, 2025
Badanie adaptogenów w leczeniu migren związanych ze stresem
Jun 26, 2025
Współpraca z lekarzem dla optymalnego zdrowia
Jul 04, 2025
Stres i bóle głowy: Zarządzanie głównym czynnikiem wyzwalającym
Jul 10, 2025
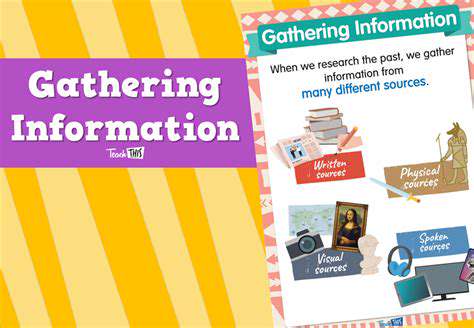
Empowerment poprzez wiedzę: Zdobycie kontroli nad migreną
Jul 16, 2025
Czy migreny to tylko silne bóle głowy? Zrozumienie rzeczywistości
Jul 20, 2025
Podejmowanie świadomych decyzji dotyczących leczenia: podejście oparte na empoweweringu
Jul 20, 2025
Łagodne rutynie fitness odpowiednie dla osób z migreną
Jul 21, 2025