Sharp Pain Behind Ear on Head: Understanding Symptoms
Table of contents
Ear infections commonly cause sharp pain behind the ear.
TMJ disorders can lead to discomfort in the ear area.
Nerve issues like trigeminal neuralgia require medical evaluation.
Physical injuries may result in sharp pain behind the ear.
Repetitive actions can strain jaw muscles, causing ear pain.
Environmental changes, such as pressure shifts, can cause discomfort.
Accompanying symptoms include headaches and dizziness with ear pain.
Tension headaches may radiate pain to the ear region.
Diagnostic approaches start with patient history and physical exams.
Home treatments include over-the-counter pain relievers and warm compresses.
Seek medical help if pain persists or accompanies concerning symptoms.
Prepare for medical visits by documenting pain intensity and triggers.
Regular follow-ups with healthcare providers enhance treatment effectiveness.
Common Causes of Sharp Pain Behind the Ear

Possible Medical Conditions
- Ear infections can lead to sharp pain behind the ear.
- Temporomandibular joint (TMJ) disorders may also cause discomfort in that region.
- Nerve-related issues, like trigeminal neuralgia, require medical assessment.
One of the most common causes of Pain Behind the Ear is ear infections. These infections can be caused by bacteria or viruses, leading to symptoms like sharp pain, swelling, and even fever. Children are particularly susceptible, but adults can experience them too. Treatment usually involves antibiotics or over-the-counter pain relievers to alleviate the discomfort.
Another medical condition to consider is a temporomandibular joint (TMJ) disorder. This issue arises from problems with the jaw and can manifest as a dull or acute pain radiating to the ear area. A proper diagnosis often requires imaging studies and may involve treatments such as dental interventions or physical therapy.
Injury and Overuse
Physical injuries to the head, neck, or jaw can also result in Sharp pain behind the ear. These injuries may include sports-related impacts or accidents that strain the muscles and tissues in that area. It's essential to get a thorough assessment to rule out fractures or more severe injuries. Rest, ice, and anti-inflammatory medications are common initial treatments.
Additionally, repetitive actions, such as chewing gum excessively or grinding teeth at night, can lead to discomfort as well. Overuse of the jaw muscles can strain the tissues and create referred pain in the ear region. Addressing habits through behavioral changes—like reducing gum chewing or seeking a mouthguard for sleep—can alleviate symptoms in many cases.
Environmental Factors
Certain environmental factors can also play a role in causing pain behind the ear. For instance, changes in air pressure, such as those experienced during flying or diving, can lead to discomfort due to fluid buildup in the ear. It's advisable to equalize pressure during flight and avoid diving with existing ear infections.
In addition, prolonged exposure to allergens or irritants can heighten sensitivity and lead to sharp pain. For those suffering from seasonal allergies, using antihistamines can be beneficial. It's crucial to identify potential triggers to prevent further episodes of pain behind the ear.
Recognizing Associated Symptoms
When to Seek Medical Attention
Understanding When Pain Becomes a Concern
Sharp pain located behind the ear can stem from various conditions, some of which may warrant immediate medical assistance. It's essential to recognize the difference between minor discomfort and symptoms signifying a more serious issue. If the pain is persistent, severe, or accompanied by other concerning symptoms, it is advisable to consult a healthcare professional.
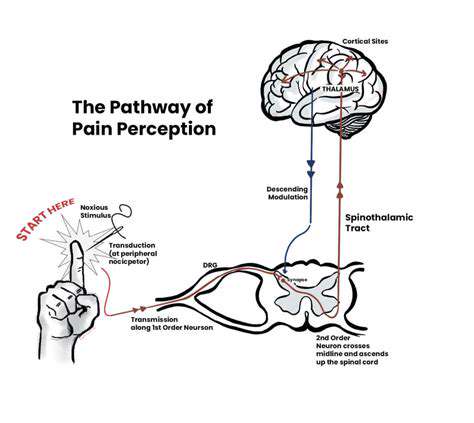
Research highlights that pain sensations often correlate with neurological issues or infections. For instance, pain behind the ear associated with fever, swelling, or changes in hearing might indicate an infection, such as mastoiditis, requiring prompt intervention to avoid complications. Always take note of accompanying symptoms to guide your decision about seeking care.
Identifying Additional Symptoms
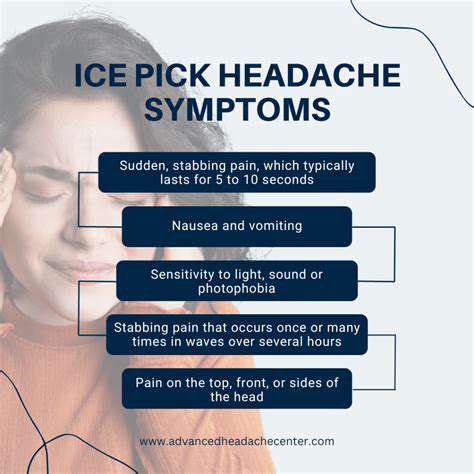
When experiencing sharp pain behind the ear, pay attention to any concurrent symptoms. This includes dizziness, numbness, visual disturbances, or severe headaches. Collectively, these symptoms can provide diagnostic clarity and should be communicated to your healthcare provider. Understanding these patterns can greatly enhance the speed and accuracy of your diagnosis.
Although some conditions can present with pain exclusively, others may involve a complex of symptoms that provide clues about the underlying problem. For example, sudden onset of dizziness might suggest vestibular issues, while vertigo might point toward inner ear disturbances. Documenting these experiences is vital for a thorough medical assessment.
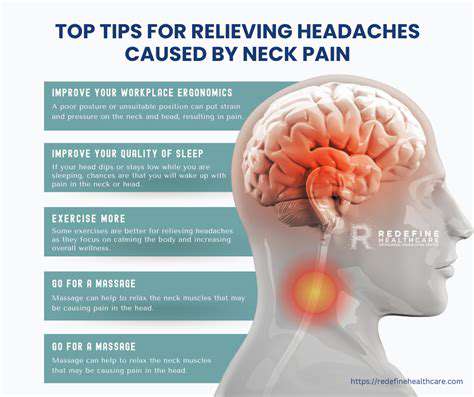
Connection to Neurological Issues
Neck pain and headaches accompanied by pain behind the ear can often signal neurological conditions. In particular, tension headaches or migraines might radiate pain to this area, complicating the clinical picture. Notably, trigeminal neuralgia, characterized by electric shock-like pain in the face, can also manifest with discomfort located around the ear region.
In rarer instances, conditions such as multiple sclerosis or even stroke may initially present with localized pain around the ear. Awareness of the potential severity of these conditions allows for more vigilant monitoring of one's symptoms, encouraging timely healthcare consultations.
When to Consider Immediate Care
Individuals should seek Immediate medical attention if the sharp pain behind the ear occurs suddenly and is associated with neurological signs like weakness, confusion, or loss of consciousness. These symptoms can indicate serious health risks, such as a stroke or other acute medical emergencies, where every minute counts for effective treatment.
Furthermore, if the pain is accompanied by a high fever, significant swelling, or fluid drainage from the ear or mouth, it could signify an urgent infection or inflammatory process. Timely assessment by a healthcare professional is crucial in these scenarios to prevent potential complications.
The Role of Family History
Family medical history is increasingly recognized as significant in evaluating conditions related to pain. If there is a known history of neurological disorders or ear problems in your family, you should inform your healthcare provider. This information can guide more tailored diagnostic and treatment approaches based on your hereditary risks.
These insights can foster a proactive approach towards better managing your health. For instance, genetic predispositions to migraines or other chronic pain conditions warrant closer monitoring and appropriate lifestyle or preventive strategies. Sharing this context empowers medical professionals to offer more personalized care options.
Preparing for Your Medical Visit
Before visiting a healthcare provider for sharp pain behind your ear, preparation can facilitate a more efficient and effective consultation. Documenting the frequency and intensity of your pain, along with any triggering activities or timelines, helps set the stage for a thorough evaluation.
Additionally, noting any medications you are taking or previous medical conditions provides your healthcare provider with enhanced context. Being equipped with this information not only aids in expediting your diagnosis but also encourages a more collaborative doctor-patient relationship.
Management and Treatment Options
Understanding the Causes of Pain Behind the Ear
Pain behind the ear can arise from various underlying conditions. One common culprit is tension headaches, which may manifest as sharp, throbbing discomfort. Stress and poor posture can contribute significantly to these headaches. It's important to note that the muscles around the neck and shoulders can tighten due to prolonged strain, resulting in referred pain that feels localized in the ear region.
Temporomandibular joint (TMJ) disorders can also lead to pain behind the ear. This joint connects the jaw to the skull and can become inflamed or misaligned. Symptoms often include clicking or popping sounds when moving the jaw, along with pain that radiates towards the ear. Addressing factors such as teeth grinding or jaw clenching, often exacerbated by stress, can mitigate TMJ-related discomfort.
Diagnostic Procedures to Identify the Cause
When experiencing sharp pain behind the ear, a thorough diagnostic approach is essential. Healthcare providers typically begin with a detailed medical history and physical examination. The aim is to assess specific symptoms and locate the pain's origin.
Certain imaging techniques, such as MRI or CT scans, may be employed to gain further insight into the internal structures of the ear and surrounding areas. These imaging methods can identify potential problems, including tumors or infections, that may require immediate intervention.
Additionally, if TMJ dysfunction is suspected, dental evaluations may include bite analysis and jaw movement assessments. This multi-faceted diagnostic approach helps ensure that treatment is appropriately directed at the underlying issue causing pain.
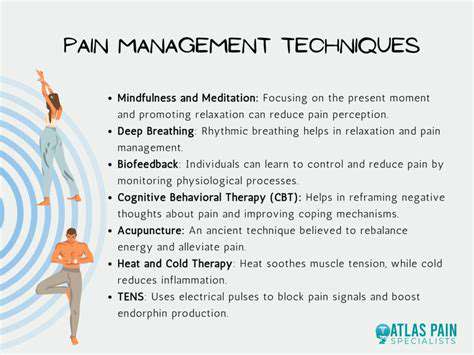
Managing Pain Through Home Remedies
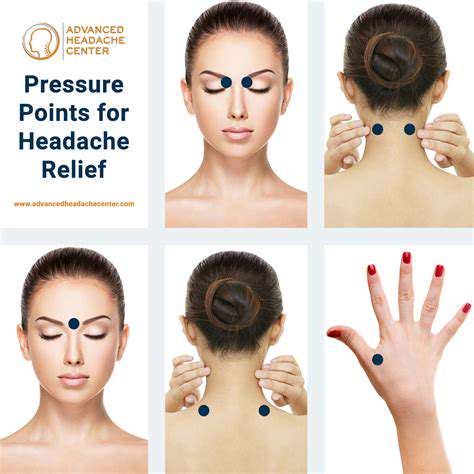
For many individuals, managing pain behind the ear can start at home. Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can provide swift relief from discomfort. Furthermore, applying a warm compress or an ice pack can soothe inflammation and reduce pain levels. Alternating between heat and cold might enhance the effectiveness of this relief strategy.
Gentle neck stretches and relaxation techniques offer additional options for managing tension-related discomfort. Incorporating practices like yoga or progressive muscle relaxation into your daily routine can address stress, a common aggravator of ear pain, while promoting overall wellbeing.
Medical Treatment Options Available
In persistent cases of ear pain that do not respond to home remedies, medical intervention may be necessary. Depending on the diagnosis, healthcare providers may prescribe medications, such as muscle relaxants for TMJ disorders or antibiotics if an infection is detected. For chronic tension headaches, preventive medications can also be explored.
In situations where physical therapy is indicated, therapists can offer specialized techniques designed to alleviate pain through targeted exercises. Patient education on posture and ergonomic adjustments may also be included as part of holistic management strategies.
Importance of Regular Follow-ups
For individuals experiencing persistent pain behind the ear, the significance of regular follow-up appointments with healthcare professionals cannot be overstated. These visits help monitor the effectiveness of treatment plans and can prompt necessary adjustments to therapy. Maintaining open communication about symptoms and any changes is crucial to developing a successful management strategy.
Moreover, for those with ongoing conditions such as TMJ, establishing a routine of check-ups can be beneficial. Early intervention often leads to better outcomes, minimizing the risk of more severe complications down the line. A collaborative approach between patients and healthcare providers ensures tailored treatment plans that evolve with the patient's needs.