Yoga Poses to Ease Tension Headaches and Migraines
Introduction to Tension Headaches and Migraines

Understanding Tension Headaches
Nearly everyone experiences tension headaches at some point, as they’re among the most common types of headaches. The discomfort typically feels like a constant, dull pressure around the forehead or back of the head, often described as a tight band squeezing the skull. Pain levels vary from mild annoyance to debilitating throbbing, sometimes lasting hours or even days. Learning to spot the early warning signs allows for quicker intervention.
What many don’t realize is how lifestyle factors directly influence headache frequency. Everyday stressors like looming deadlines or family conflicts frequently trigger episodes. Even seemingly harmless habits – hunching over phones for hours or skipping meals – can set the stage for pain. Keeping a symptom diary helps identify personal triggers before they escalate.
Causes and Risk Factors
Medical researchers continue investigating why some people develop tension headaches while others don’t. What’s clear is that multiple factors converge to create the perfect storm. Workplace demands that cause prolonged computer use frequently lead to strained neck muscles and subsequent headaches. Interestingly, even emotional stress manifests physically through clenched jaw muscles and tightened shoulder muscles. Dehydration and sleep deprivation compound these effects, making headaches more likely.
Certain groups face higher risks than others. Office workers maintaining static postures for hours report more frequent headaches. Students facing exam pressure often experience cyclical headache patterns. Women tend to report more tension headaches than men, possibly due to hormonal influences or societal stress factors. Recognizing these risk factors enables better prevention strategies.
Symptoms and Diagnosis
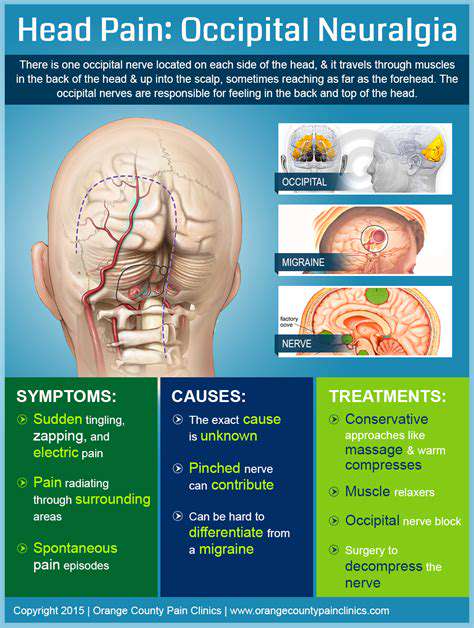
The classic tension headache presents as bilateral pressure – imagine wearing a helmet two sizes too small. Unlike migraines, these headaches rarely cause light sensitivity or vomiting, though some report mild nausea. Many patients describe peculiar sensations like scalp tenderness or feeling their hair hurts when touched. Doctors typically diagnose based on symptom patterns rather than complex tests, though persistent cases may require imaging to rule out other conditions.
Treatment and Management
Most tension headaches respond well to basic interventions. Over-the-counter medications like aspirin or naproxen provide relief for many, though medication overuse can ironically trigger rebound headaches. What truly makes the difference is addressing root causes through comprehensive lifestyle changes. Simple adjustments like scheduled screen breaks, ergonomic workspace setups, and regular hydration often yield dramatic improvements.
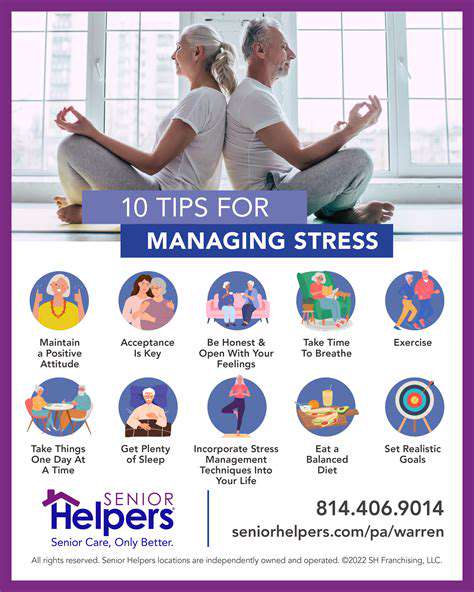
Mind-body techniques deserve special attention. Progressive muscle relaxation systematically releases tension from toes to scalp. Biofeedback training helps patients recognize and control physical stress responses. Even brief midday meditation sessions can interrupt the stress-headache cycle. Combined with regular aerobic exercise and consistent sleep patterns, these approaches form a powerful defense against chronic tension headaches.
Shoulder and Upper Back Opening Poses

Shoulder and Upper Back Flexibility
Modern lifestyles wreak havoc on upper body mobility, with hours spent hunched over devices creating chronic tightness. This postural strain frequently manifests as nagging discomfort between shoulder blades or limited arm rotation. Targeted mobility work not only relieves existing stiffness but prevents future movement restrictions. The key lies in consistent, gentle practice rather than aggressive stretching.
Specific attention to postural muscles yields disproportionate benefits. The rhomboids between shoulder blades particularly suffer from prolonged sitting, leading to rounded shoulders. The trapezius muscles spanning neck and shoulders accumulate tension from stress. Even the small levator scapulae muscles connecting neck to shoulder blades contribute to discomfort when overworked. Addressing these areas systematically restores natural movement patterns.
Importance of Posture
Posture affects far more than appearance – it influences breathing efficiency, digestion, and even mood states. Chronic slumping compresses internal organs and strains spinal discs, while proper alignment optimizes bodily functions. Conscious posture maintenance literally changes how the body processes stress, reducing cortisol levels over time. The mental benefits prove equally significant, with upright postures correlating with increased confidence and positive affect.
True postural improvement requires whole-body awareness. It’s not just about pulling shoulders back, but aligning ears over shoulders, ribs over pelvis, and maintaining neutral spinal curves. Micro-adjustments throughout the day – like elevating computer monitors or using lumbar support – make sustained improvement possible. The cumulative effect of these small changes significantly reduces musculoskeletal strain.
Exercises for Improved Mobility
Effective mobility routines address multiple movement planes. While simple neck rolls provide temporary relief, comprehensive programs yield lasting change. Scapular stabilization exercises often produce dramatic improvements, as weak supporting muscles force larger muscles to overwork. Rotator cuff strengthening prevents the shoulder impingement that frequently accompanies poor posture.
Accessible exercises deliver surprising benefits. Wall angels (sliding arms up and down while maintaining contact) improve shoulder range of motion. Thread-the-needle stretches open tight chest muscles. Even basic chin tucks counter forward head posture. Performed consistently, these movements re-educate the body toward healthier movement patterns, reducing pain and stiffness over weeks and months.
Prevention and Management of Pain
Breaking the pain cycle requires addressing both symptoms and causes. While massage and heat therapy provide temporary relief, lasting improvement comes from changing daily habits. Ergonomic assessments often reveal simple fixes – raising chairs, adjusting keyboard height, or using standing desks intermittently. These modifications prevent the repetitive strain that underlies chronic discomfort.
Active recovery methods prove most effective. Contrast hydrotherapy (alternating heat and cold) reduces inflammation while improving circulation. Self-myofascial release using foam rollers breaks up muscular adhesions. Perhaps most importantly, scheduled movement breaks every 30-60 minutes prevent stiffness from setting in. This proactive approach maintains mobility and prevents minor discomfort from becoming debilitating pain.
Deep Breathing Techniques for Headache Relief
Diaphragmatic Breathing
Diaphragmatic breathing serves as nature’s tranquilizer, activating the parasympathetic nervous system. This fundamental technique counters the shallow chest breathing that accompanies stress. By consciously expanding the abdomen during inhalation, practitioners increase oxygen exchange while stimulating the vagus nerve. This nerve acts as the body’s natural calming circuit, slowing heart rate and reducing muscle tension – particularly beneficial for tension headache sufferers.
Mastering this technique requires patience. Beginners often mistakenly lift their shoulders, engaging accessory breathing muscles instead of the diaphragm. A helpful visualization imagines the abdomen as a balloon inflating with each inhale, deflating with each exhale. Placing a light book on the stomach provides tactile feedback – the book should rise and fall with each breath. Regular practice makes this pattern automatic, creating an always-available tool for headache prevention.
Box Breathing
Box breathing, or square breathing, offers military-grade stress reduction in a simple package. Navy SEALs use this technique to maintain composure in high-stress situations, and it works equally well for headache management. The equal-length phases create a meditative rhythm that disrupts anxious thought patterns. This method particularly helps those whose headaches stem from work stress or emotional tension.
The beauty lies in its adaptability. While the classic 4-4-4-4 pattern works well, individuals can adjust counts to their comfort level. Some find extending the exhale (perhaps 4-4-6-4) enhances relaxation. The brief breath holds after inhalation oxygenate tissues more thoroughly, while post-exhalation holds allow complete carbon dioxide release. Practiced consistently, this technique can lower baseline stress levels, reducing headache frequency over time.
Restorative Poses and Relaxation

Deep Relaxation and Stillness
Restorative yoga offers an antidote to modern hyperactivity, creating space for nervous system recovery. These supported poses differ dramatically from active yoga styles, requiring minimal muscular engagement. The magic happens through prolonged, passive stretching that allows connective tissues to release gradually. This approach proves particularly valuable for headache sufferers holding tension in neck and shoulder muscles.
Proper prop usage transforms these poses. Strategically placed bolsters support the spine in gentle extension, while folded blankets cushion bony prominences. Eye pillows block visual stimuli, enhancing relaxation. The resulting state resembles the twilight between wakefulness and sleep, where healing processes activate most effectively. Even 10-15 minutes in these positions can reset an overtaxed nervous system.
Legs Up the Wall and Savasana
Legs-up-the-wall pose (Viparita Karani) provides profound benefits with minimal effort. This gentle inversion reverses blood flow patterns, reducing lower extremity swelling while calming the nervous system. Many practitioners report this pose particularly alleviates headaches stemming from neck tension or poor circulation. The passive nature makes it accessible even to those with limited mobility.
Savasana (corpse pose) represents the culmination of practice, yet many underestimate its power. True Savasana involves complete surrender – not just physical stillness but mental release. This conscious rest state allows the body to integrate the benefits of preceding poses while lowering stress hormone levels. For headache sufferers, mastering this art of conscious relaxation often proves more valuable than any medication.