HTML
CSS
HTML element
CSS class
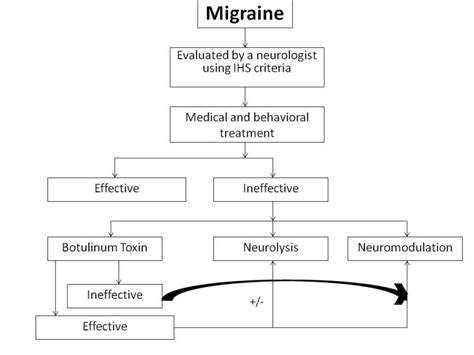
Migraine
MSG
MSG(グルタミン酸ナトリウム)が潜在的な片頭痛誘発物質として
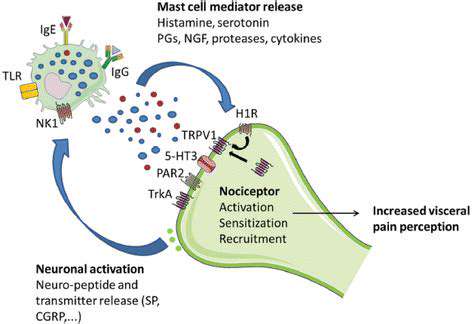
MSG誘発性頭痛の可能性のあるメカニズム
潜在的な細胞メカニズム
グルタミン酸ナトリウム (MSG) は、加工食品によく使用される味覚増強剤であり、議論を巻き起こしています。
MSGが片頭痛を引き起こす要因に関する研究と証拠
Read more about MSG(グルタミン酸ナトリウム)が潜在的な片頭痛誘発物質として
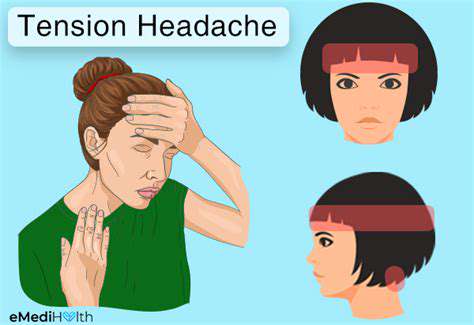
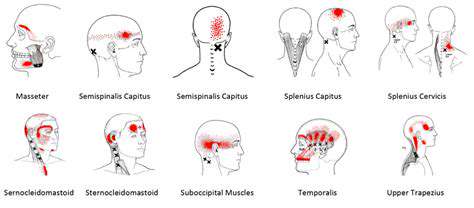
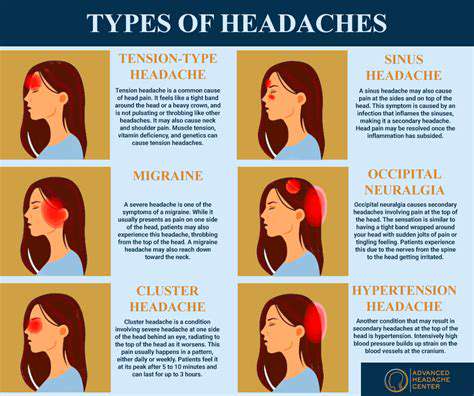
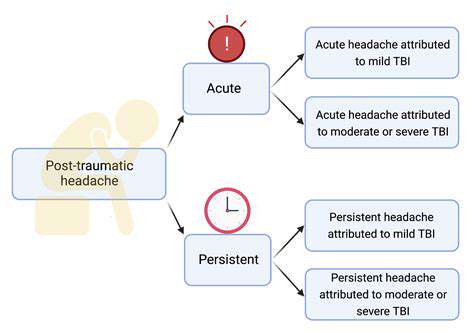
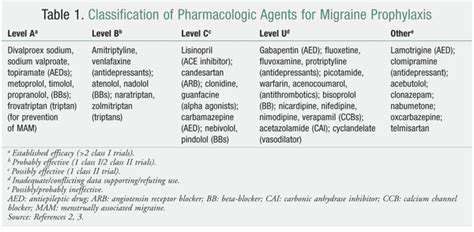
一般的な頭痛の理解と管理。緊張型頭痛、副鼻腔炎、偏頭痛、眼精疲労を含む一般的な頭痛タイプを管理するための効果的な戦略を発見してください。最も一般的な形式である緊張型頭痛は、しばしばストレスや筋肉の緊張から派生し、額周囲に鈍く締め付ける感覚として現れます。症状を特定し、原因を認識し、不快感を軽減するためのさまざまな治療オプションを探索する方法を学びましょう。顔の痛みと圧迫感が特徴の副鼻腔炎は、感染やアレルギーから起こる可能性があります。合併症を予防するために、タイムリーな診断とカスタマイズされた治療計画の重要性を理解してください。さらに、激しい脈動性の痛みと悪心のような追加症状で特徴付けられる偏頭痛の発作について深く掘り下げ、それらの頻度と重症度を管理するための急性および予防治療を探検してください。眼精疲労は、特に長時間の画面使用の後に頭痛を伴うことがあります。20-20-20 ルール、画面調整、適切な照明などの実用的なヒントで緩和策を見つけてください。緊張型頭痛やその他の頭痛関連の状態に対処している場合、この包括的なガイドは、症状認識、生活様式の調整、医療相談を求めるタイミングについて貴重な洞察を提供します。---*頭痛を効果的に管理し、生活の質を取り戻しましょう!*
Jan 07, 2025