Vergelijking van neuromodulatietoestellen voor migraine
Neuromodulatie is een fascinerend gebied dat diverse technieken omvat die gericht zijn op het veranderen van de activiteit van neuronale circuits in de hersenen en het lichaam. Deze verfijnde aanpak biedt een niet-invasieve of minimaal invasieve manier om een breed scala aan neurologische aandoeningen te behandelen.
Transcraniële magnetische stimulatie (TMS) voor de preventie van migraine
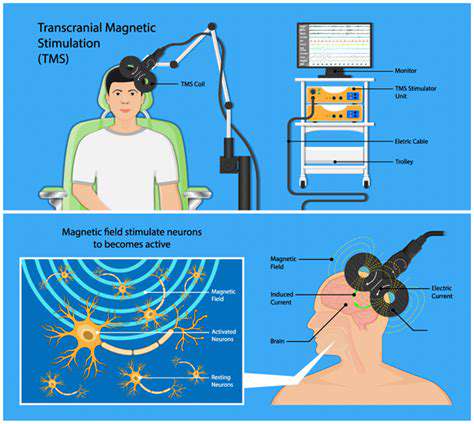
Principes van transcraniële magnetische stimulatie (TMS)
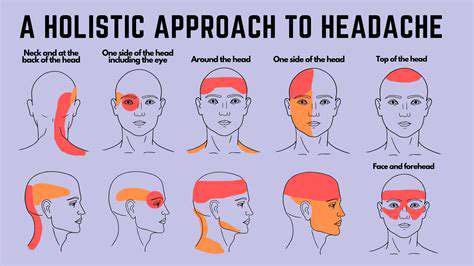
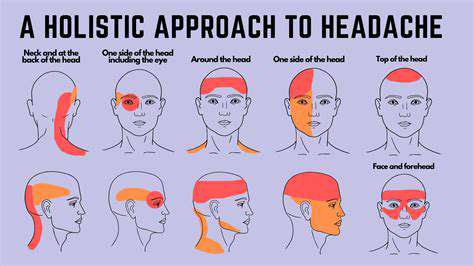
Transcraniële magnetische stimulatie (TMS) is een niet-invasieve behandeling die magnetische pulsen gebruikt om specifieke hersengebieden te stimuleren. Het doel is om de activiteit van de hersenen te beïnvloeden en zo de frequentie en ernst van migraine aanvallen te verminderen. De stimulatie wordt toegepast op het hoofd, doorgaans op de hersenschors die betrokken is bij de pijnsignalering en de regulatie van de bloedvaten. De exacte mechanismen die hierachter liggen, zijn nog steeds onderwerp van onderzoek, maar de behandeling vertoont veelbelovend potentieel voor patiënten die lijden aan chronische migraine.
Stimulatie van de Nervus Vagus (VNS) bij Chronische Migraine

Begrijpen van de Nervus Vagus
De nervus vagus Migrainepatiënten ervaren vaak een complexe wisselwerking van factoren die aanvallen van invaliderende hoofdpijn kunnen veroorzaken. Het identificeren van deze triggers is essentieel voor het effectief
Periphere zenuwstimulatie voor migraine-uitlokkende pijn
Migraine-triggers begrijpen