Neuroscience
Medical_treatment
Brain Stimulation
Nervous System
Physiology
HTML
CSS
Headaches
Pain Management
比較神經調控設備治療偏頭痛
廣泛概述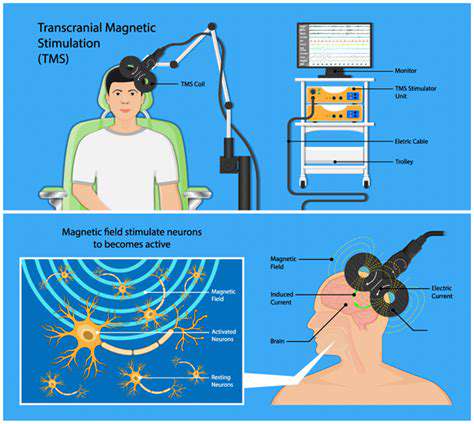

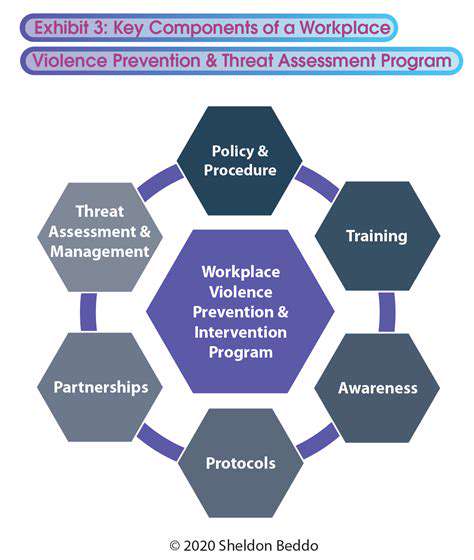
神經調控是一個引人入勝的領域,涵蓋各種旨在改變大腦和身體神經迴路活動的技術。這種先進的方法提供了一種非侵入性或微創的方法來治療廣泛...
顱內磁刺激 (TMS) 預防偏頭痛
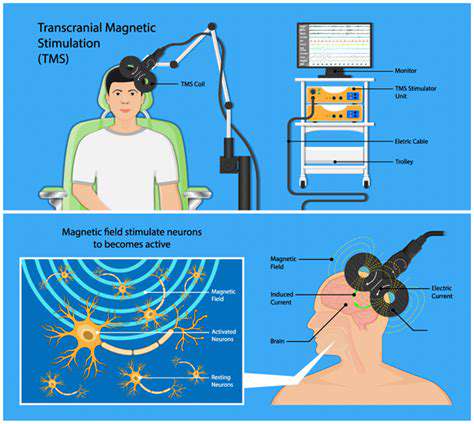
顱內磁刺激 (TMS) 原理
顱內
迷走神經刺激療法 (VNS) 治療慢性偏頭痛

Read more about 比較神經調控設備治療偏頭痛
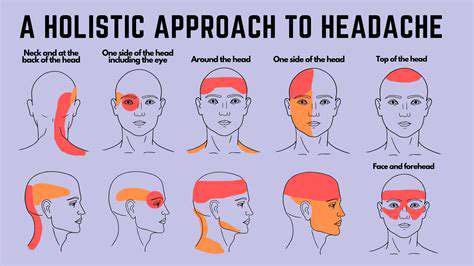
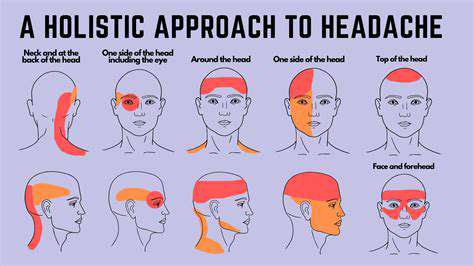
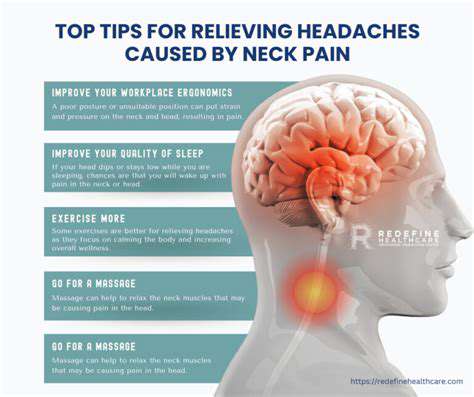
症狀、原因和治療頭皮疼痛的症狀可以從鈍痛到尖銳的刺痛感不等,影響日常活動和整體健康。及早識別如觸痛或伴隨的頭痛等症狀對於有效管理至關重要。頭皮疼痛的潛在原因差異很大,包括緊張性頭痛、如銀屑病等頭皮疾病或如枕神經痛等神經問題。有效的治療策略包括非處方止痛藥、針對炎症的局部解決方案以及針對持續性問題的專業諮詢。本全面指南概述了常見症狀、潛在原因和治療選擇,幫助個人有效管理頭皮疼痛。探索維持頭皮健康的整體方法,包括壓力管理技巧、營養豐富的飲食和定期與醫療服務提供者的檢查。優先考慮你的頭皮健康可以帶來無痛、充滿活力的生活。
Nov 12, 2024
了解頭皮疼痛的常見原因,並探索有效的治療方案。我們的綜合指南涵蓋從偏頭痛和緊張性頭痛到頭皮狀況(如牛皮癬)和神經相關疼痛的所有內容。學習識別症狀的重要性、管理潛在疾病,並利用藥物和家庭療法來緩解不適。透過生活方式的改變提升您的福祉,並尋求針對頭皮健康的量身定制解決方案。今天就獲取情報,緩解持續性頭皮疼痛!
Nov 22, 2024
在我們關於疼痛結的啟發性文章中,探索壓力、創傷與身體疼痛之間的複雜聯繫。了解情感壓力如何引發肌肉緊張,從而導致不適,並發現一些有效的緩解策略,包括正念、按摩療法和身體實踐。深入了解識別疼痛結的症狀和原因,並理解何時需要專業幫助。通過實用技巧和長期解決方案,賦予自己培養更健康的身心連接,以征服疼痛的循環。解開您不適背後的情感因素,擁抱整體健康的方法。
Dec 07, 2024
疼痛可能源自神經、血管、肌肉、鼻竇或下顎問題。- 症狀識別:症狀包括搏動性疼痛、對光敏感、噁心和視覺障礙。記錄症狀日記有助於診斷。- 治療選擇:治療因病因而異,可能包括非處方藥、生活方式改變和針灸等替代療法。症狀與類型- 常見症狀:鈍痛、尖銳痛、搏動感和壓迫感。伴隨症狀可能包括對光和聲音的敏感性。- 偏頭痛與頭痛:偏頭痛是右側頭痛的主要原因,伴隨光敏感和噁心。其他類型包括緊張性頭痛和叢集性頭痛。管理策略- 家庭療法:冷敷和非處方藥可以提供即時緩解。專注於水分攝取、飲食和睡眠的生活方式變化對預防至關重要。- 專業護理:對於持續性疼痛,諮詢醫療專業人員是必不可少的。專門的治療可能包括處方藥、物理治療或認知行為療法。結論:了解右側頭痛的原因、症狀和治療選擇對於有效管理至關重要。早期介入可以提高生活質量並減少不適。對於個性化護理,始終諮詢醫療提供者。若需更詳細的見解,請查閱我們關於右側頭痛的深入文章。
Jan 13, 2025
探索右側頭痛的原因和管理方法,了解肌肉緊張、鼻竇問題和偏頭痛等潛在原因。我們的綜合指南提供有關常見誘因、壓力影響和需注意的嚴重病症的見解。學習何時尋求醫療幫助,探索有效的管理選項和家庭療法以緩解不適。了解主動健康措施,如諮詢醫療專業人士,如何幫助解決潛在原因,為那些尋求右側頭痛緩解的人提供一站式資源。
Jan 13, 2025
理解右側頭痛及其管理探索右側頭痛的常見誘因和症狀,包括緊張、飲食因素和環境影響。了解與這種疼痛相關的潛在醫學狀況,如偏頭痛和鼻竇感染,並學會何時尋求急診護理。我們的綜合指南概述了有效的管理策略,包括生活方式的改變、減壓技巧和醫療治療選擇。增強自己的知識,識別誘因並實施長期預防策略,以改善生活質量。訪問我們,深入了解右側頭痛的診斷和治療。
Jan 19, 2025
理解肌肉緊張和頭痛的生理學描述:在我們的綜合指南中,發現肌肉緊張與頭痛之間錯綜複雜的關係。了解壓力、不良姿勢和生活方式選擇如何導致肌肉緊繃和緊張性頭痛。探索有效的治療方法,包括物理療法、放鬆技巧,以及結合傳統與整體實踐的綜合方法。尋找實際解決方案以緩解肌肉緊張、管理頭痛症狀,並改善整體健康。告別慢性頭痛,擁抱更健康的生活方式。
Feb 25, 2025