Comparing Neuromodulation Devices for Migraine
Neuromodulation is a fascinating field encompassing various techniques aimed at altering the activity of neuronal circuits in the brain and body. This sophisticated approach offers a non-invasive or minimally invasive way to treat a wide range of neurological and psychiatric disorders. It manipulates the nervous system, influencing the communication between neurons and ultimately impacting behavior and physiology. This process differs from direct stimulation, which often targets specific neurons for activation, whereas neuromodulation focuses on modifying the overall communication network.
Types of Neuromodulation Techniques
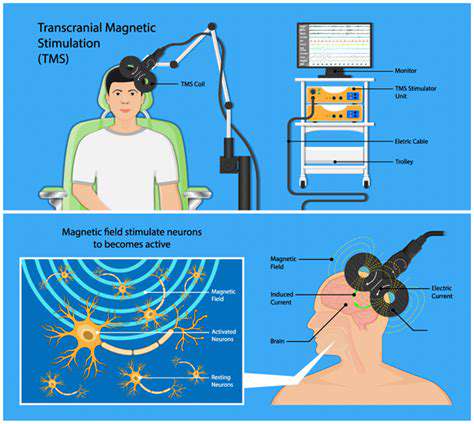
Several distinct neuromodulation techniques exist, each employing different mechanisms to achieve their therapeutic goals. Transcranial magnetic stimulation (TMS) uses magnetic pulses to induce electrical currents in the brain, while deep brain stimulation (DBS) involves implanting electrodes deep within the brain to deliver electrical pulses. These techniques offer a targeted approach to specific neurological conditions. Other methods include vagus nerve stimulation (VNS) and transcranial direct current stimulation (tDCS), each with unique mechanisms and applications.
Mechanism of Action and Target Areas
Understanding the precise mechanisms of neuromodulation is crucial for optimizing treatment strategies. The impact on specific brain regions and pathways varies depending on the technique used. For instance, TMS primarily affects cortical areas, whereas DBS can target deeper brain structures like the basal ganglia. Understanding these targeted areas helps clinicians tailor treatment plans to individual patient needs. Furthermore, the interplay between neurotransmitters and neuromodulatory pathways plays a significant role in the therapeutic effects of these interventions.
Applications in Neurological and Psychiatric Disorders
Neuromodulation has emerged as a promising therapeutic option for a spectrum of neurological and psychiatric disorders. Conditions like Parkinson's disease, depression, and epilepsy show substantial potential for improvement using these techniques. The non-invasive nature of some techniques makes them attractive options for patients who may not be suitable candidates for invasive procedures. Moreover, the ability to modulate specific neural pathways allows for a more precise and targeted approach to treatment.
Safety and Efficacy Considerations
While neuromodulation offers significant therapeutic potential, safety and efficacy remain critical considerations. Careful patient selection and rigorous monitoring are essential to minimize potential side effects. Potential complications vary depending on the specific technique used, and understanding these risks is critical for informed decision-making. Long-term outcomes and efficacy rates also require further investigation to fully assess the long-term benefits of these interventions. Clinical trials and ongoing research play a crucial role in refining and validating these techniques.
Future Directions and Research
The future of neuromodulation is bright, with ongoing research exploring new techniques and applications. Development of more sophisticated targeting methods and personalized treatment protocols is crucial. Advancements in neuroimaging and neurotechnology promise to enhance our understanding of the brain's intricate workings and pave the way for more precise and effective neuromodulation therapies. This field holds immense potential to revolutionize the treatment of neurological and psychiatric disorders, ultimately improving the lives of countless individuals.
Transcranial Magnetic Stimulation (TMS) for Migraine Prevention
Transcranial Magnetic Stimulation (TMS) Principles
Transcranial magnetic stimulation (TMS) is a non-invasive brain stimulation technique that uses magnetic pulses to induce electrical currents in specific brain regions. These magnetic pulses are delivered through a coil placed on the scalp, targeting the desired area of the brain. TMS has become a valuable tool for both research and clinical applications, providing insights into brain function and potential therapeutic interventions. The technology works by creating a rapidly changing magnetic field, which induces electrical currents in the underlying neural tissue.
The strength and duration of the magnetic pulses, as well as the location and timing of stimulation, can be precisely controlled. This allows researchers and clinicians to selectively activate or inhibit specific neuronal populations, enabling investigation into the role of different brain regions in various cognitive functions and neurological disorders. This precise control is a key advantage over other brain stimulation techniques.
TMS Applications in Neuroscience Research
TMS has revolutionized neuroscience research by enabling researchers to study the causal relationship between brain activity and behavior. By stimulating or inhibiting specific brain regions, researchers can observe the corresponding effects on cognitive processes, such as memory, language, and motor control. This causal approach allows for a deeper understanding of the neural mechanisms underlying these functions.
Furthermore, TMS can be used to study the plasticity of the brain, investigating how the brain adapts and reorganizes itself in response to experience or injury. This is particularly valuable in understanding recovery processes following stroke or traumatic brain injury. By combining TMS with other neuroimaging techniques, researchers can gain a comprehensive picture of brain function and dysfunction.
TMS Clinical Applications and Safety
Beyond research, TMS is increasingly used in clinical settings for treating various neurological and psychiatric conditions. For example, it has shown promise in the treatment of major depressive disorder, obsessive-compulsive disorder, and other conditions. The precise mechanisms by which TMS exerts its therapeutic effects are still being investigated, but the results are encouraging and offer new hope for patients struggling with these conditions.
TMS is generally considered a safe procedure when performed by qualified professionals. However, potential side effects, such as mild headaches or muscle twitching, can occur. Strict safety protocols and careful monitoring are essential to minimize these risks. The overall safety profile of TMS is generally favorable, making it a valuable tool for treating neurological and psychiatric conditions.
Vagus Nerve Stimulation (VNS) for Chronic Migraine Management

Understanding the Vagus Nerve
The vagus nerve is a crucial part of the parasympathetic nervous system, playing a vital role in regulating various bodily functions, including heart rate, digestion, and breathing. Its extensive network throughout the body makes it a complex and important component of overall health. Understanding its function is key to comprehending the mechanisms behind VNS.
This complex nerve, with its branches extending to multiple organs, plays a significant role in the body's overall homeostasis. It helps maintain balance and coordinate various physiological processes. It's a vital part of the body's intricate communication system.
The Role of VNS in Treating Neurological Conditions
VNS is a neurostimulation therapy that targets the vagus nerve to potentially alleviate symptoms of certain neurological disorders. By electrically stimulating this nerve, it's hoped that the brain's activity can be modulated, potentially leading to improved outcomes for patients. This procedure has shown promise in managing conditions like epilepsy and depression.
VNS therapy aims to alter the abnormal electrical activity in the brain that contributes to these conditions. It's a non-invasive intervention for patients who haven't found other treatments effective.
How VNS Works
A small device, known as a neurostimulator, is surgically implanted under the skin in the chest. This device delivers electrical pulses to the vagus nerve, thereby influencing its activity and potentially affecting the brain's activity. This stimulation can help regulate the brain's electrical signals and potentially reduce symptoms.
The pulses generated by the device are carefully calibrated to avoid adverse effects while stimulating the vagus nerve to achieve the desired therapeutic outcome.
Types of Conditions Treatable with VNS
VNS is primarily used to treat epilepsy, particularly when other treatments have proven ineffective. It can also be explored as a potential treatment for severe depression. These conditions often involve complex neurological processes, making VNS a potential therapeutic option.
Surgical Procedure and Implantation
The surgical procedure for implanting the VNS device is generally considered safe and effective. A neurosurgeon performs the procedure, implanting the device in the chest wall. The device is programmed to deliver specific electrical pulses, carefully tailored to the individual patient's needs.
Post-operative care is crucial to ensure proper healing and minimize complications. Regular follow-up appointments with the healthcare team are essential to monitor the device's functioning and adjust settings as needed.
Potential Side Effects and Risks
While generally safe, VNS, like any medical procedure, carries potential side effects. These can include hoarseness, voice changes, and dysphagia (difficulty swallowing). Careful monitoring is essential to manage any potential complications and ensure the patient's well-being.
Patients should discuss potential side effects with their healthcare team before undergoing VNS therapy.
Effectiveness and Long-Term Outcomes
The effectiveness of VNS varies from patient to patient. Some experience significant symptom reduction, while others may not find the treatment as helpful. Long-term outcomes are influenced by factors such as the condition being treated and the individual's response to the therapy.
Regular follow-up care and adjustments to the device's settings are often necessary to optimize results over time.
Peripheral Nerve Stimulation for Migraine Triggering Pain
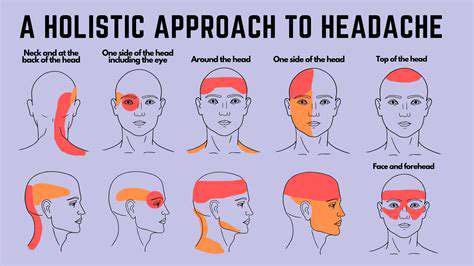
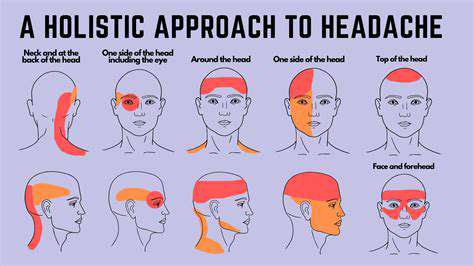
Understanding Migraine Triggers
Migraine sufferers often experience a complex interplay of factors that can trigger debilitating headaches. Identifying these triggers is crucial for effective pain management. Understanding the specific stimuli that initiate a migraine attack, from environmental changes to dietary choices and even emotional stressors, can empower individuals to take proactive steps to minimize their frequency and intensity. This knowledge allows for a personalized approach to managing migraine, moving beyond a one-size-fits-all approach and towards targeted interventions.
Triggers can be diverse and range from specific foods and odors to changes in weather patterns and even stress levels. Recognizing these patterns through detailed tracking and journaling is often essential for understanding one's own unique sensitivities and developing strategies for mitigation.
The Role of Nociceptive Pathways
Nerve impulses, or nociception, play a vital role in transmitting pain signals to the brain. These signals originate from various parts of the body, including the head and neck. In migraine, these pathways become sensitized, leading to an amplified perception of pain. This sensitization can be influenced by a variety of factors, including underlying inflammation and neurochemical imbalances, making the process of pain perception more complex than a simple signal transmission.
Peripheral Nerve Stimulation: A Neuromodulatory Approach
Peripheral nerve stimulation (PNS) is a neuromodulatory technique that aims to interrupt the pain signals traveling along peripheral nerves. By applying targeted electrical or other stimuli to these nerves, PNS seeks to alter the way the nervous system processes pain, potentially reducing the intensity and frequency of migraine attacks. This approach addresses the source of the pain signals rather than simply treating the symptoms.
This method involves precisely stimulating specific nerves, potentially re-calibrating the way the body reacts to pain signals. The goal is to establish a new baseline for pain perception, reducing the sensitivity and intensity of migraine-related pain impulses.
Mechanisms of Action in Migraine Relief
The mechanisms behind PNS in migraine relief are multifaceted and not fully understood. However, it's believed that stimulation can influence the release of neurotransmitters, impacting pain signal transmission. This modulation of neurochemical activity within the nervous system aims to reduce the intensity and duration of migraine attacks. Further research is crucial for a complete understanding of the intricate pathways involved.
Comparing PNS with Other Neuromodulation Techniques
Neuromodulation encompasses a range of techniques aimed at altering the nervous system's response to pain. Techniques like transcranial magnetic stimulation (TMS) and spinal cord stimulation (SCS) also fall under this category. PNS, however, focuses specifically on the peripheral nerves, offering a different approach to managing pain compared to strategies that target the brain or spinal cord. Understanding the distinctions between these methods is essential for selecting the most appropriate intervention for individual patients.
Comparative studies are needed to definitively establish the efficacy and safety profiles of each approach in managing various types of chronic pain, including migraine.
Safety and Potential Side Effects of PNS
While generally considered safe, PNS, like any medical procedure, comes with potential side effects. These side effects can vary from mild discomfort at the stimulation site to more significant complications. Careful monitoring and evaluation by healthcare professionals are essential to manage any adverse reactions and ensure patient safety. A detailed discussion of potential complications and their management strategies is crucial for informed decision-making.
Patient education and thorough pre-procedure assessments are vital to minimize risks and maximize the benefits of PNS therapy in managing migraine-related pain.