Neuroscience
Medical_treatment
Brain Stimulation
Nervous System
Physiology
HTML
CSS
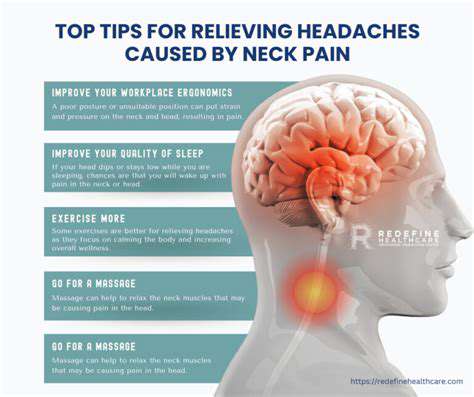
Headaches
Pain Management
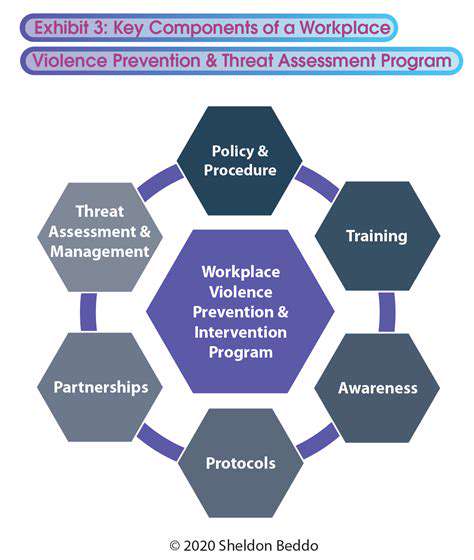
Comparando Dispositivos de Neuromodulação para Migraña
Uma Visão Geral Ampla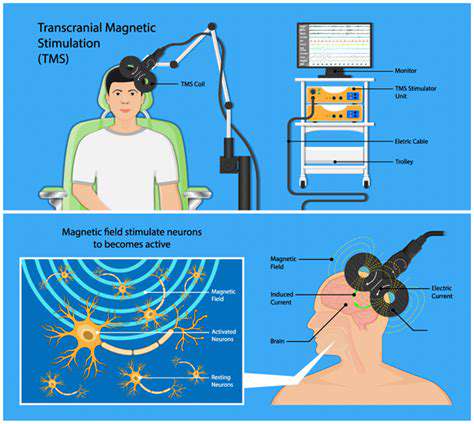

A neuromodulação é um campo fascinante que engloba várias técnicas destinadas a alterar a atividade dos circuitos neurais no cérebro e no corpo. Esta abordagem sofisticada oferece uma forma não invasiva ou minimamente invasiva de tratar uma ampla gama de
Estimulação Magnética Transcraniana (TMS) para Prevenção de Enxaqueca
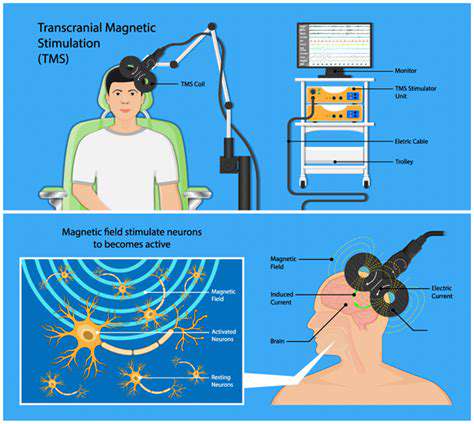
Princípios da Estimulação Magnética Transcraniana (TMS)
Estimulação magnética transcraniana
Estímulo do Nervo Vago (VNS) para o Manejo da Migraine Crônica

Compreendendo o Nervo Vago
O Pacientes com enxaqueca frequentemente experimentam uma complexa interação de fatores que podem desencadear dores de cabeça debilitantes. Identificar esses gatilhos é crucial para
Estímulo Nervoso Periférico para Dor Provocadora de Enxaquecas
Compreendendo os Gatilhos da Enxaqueca
Read more about Comparando Dispositivos de Neuromodulação para Migraña
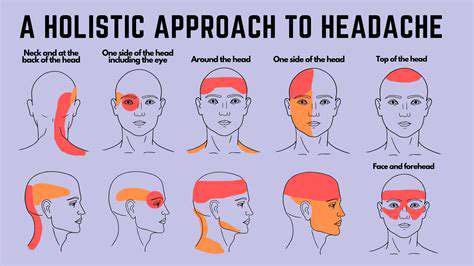
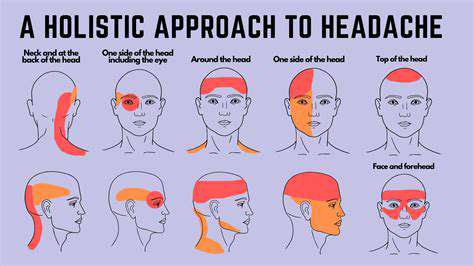
Sintomas, Causas e TratamentosA dor no couro cabeludo pode variar de uma dor maçante a sensações agudas e perfurantes, afetando as atividades diárias e o bem-estar geral. Reconhecer sintomas como sensibilidade ou dores de cabeça associadas precocemente é crucial para um gerenciamento eficaz. As causas potenciais da dor no couro cabeludo variam amplamente, incluindo dores de cabeça tensionais, condições do couro cabeludo como psoríase ou problemas nervosos como a neuralgia occipital. Estratégias de tratamento eficazes incluem analgésicos de venda livre, soluções tópicas para inflamação e consultas profissionais para problemas persistentes. Este guia abrangente descreve os sintomas comuns, causas potenciais e opções de tratamento para ajudar os indivíduos a gerenciar sua dor no couro cabeludo de forma eficaz. Explore abordagens holísticas para manter a saúde do couro cabeludo, incluindo técnicas de manejo do estresse, dietas ricas em nutrientes e verificação regular com provedores de saúde. Priorizar a saúde do couro cabeludo pode levar a uma vida vibrante e livre de dor.
Nov 12, 2024
Descubra as causas comuns da dor no couro cabeludo e explore opções de tratamento eficazes. Nosso guia abrangente cobre tudo, desde enxaquecas e dores de cabeça tensionais até condições do couro cabeludo como psoríase e dor relacionada a nervos. Aprenda sobre a importância de reconhecer os sintomas, gerenciar condições subjacentes e utilizar medicamentos e remédios caseiros para aliviar o desconforto. Melhore seu bem-estar com mudanças no estilo de vida e procure soluções personalizadas para a saúde do couro cabeludo. Informe-se e encontre alívio da dor persistente no couro cabeludo hoje mesmo!
Nov 22, 2024
Explore as conexões intrincadas entre estresse, trauma e dor física em nosso artigo esclarecedor sobre nodos dolorosos. Aprenda como o estresse emocional provoca tensão muscular, resultando em desconforto, e descubra estratégias eficazes para alívio, incluindo mindfulness, terapia de massagem e práticas somáticas. Ganhe insights sobre como identificar os sintomas e causas dos nodos dolorosos e entenda quando pode ser necessária ajuda profissional. Capacite-se com técnicas práticas e soluções de longo prazo para cultivar uma conexão mente-corpo mais saudável e conquistar os ciclos de dor. Desvenda os componentes emocionais por trás do seu desconforto e abrace uma abordagem holística para o bem-estar.
Dec 07, 2024
A dor pode originar-se de nervos, vasos sanguíneos, músculos, seios paranasais ou problemas na mandíbula. - Identificação dos Sintomas: Os sintomas incluem dor pulsante, sensibilidade à luz, náusea e distúrbios visuais. Manter um diário de sintomas ajuda no diagnóstico. - Opções de Tratamento: O tratamento varia conforme a causa e pode incluir medicamentos de venda livre, mudanças de estilo de vida e terapias alternativas como acupuntura. Sintomas e Tipos - Sintomas Comuns: Dores surdas, dores agudas, sensações pulsantes e sentimentos de pressão. Sintomas acompanhantes podem incluir sensibilidade à luz e sons. - Enxaqueca e Cefaleias: As enxaquecas são uma das principais causas de dor na lateral direita da cabeça, acompanhadas de sensibilidade à luz e náusea. Outros tipos incluem cefaleias tensionales e em clusters. Estratégias de Manejo - Remédios Caseiros: Compressas frias e medicamentos de venda livre podem proporcionar alívio imediato. Mudanças no estilo de vida focadas na hidratação, dieta e sono são vitais para a prevenção. - Cuidados Profissionais: Para dor persistente, consultar profissionais de saúde é essencial. Tratamentos especializados podem incluir medicamentos de prescrição, fisioterapia ou terapia cognitivo-comportamental. Conclusão: Entender as causas, sintomas e opções de tratamento da dor na lateral direita da cabeça é vital para o gerenciamento eficaz. A intervenção precoce pode melhorar a qualidade de vida e reduzir o desconforto. Para cuidados personalizados, consulte sempre um profissional de saúde. Para mais informações detalhadas, explore nossos artigos aprofundados sobre dor na lateral direita da cabeça.
Jan 13, 2025
Explorando as Causas e Gestão da Dor de Cabeça do Lado Direito. Descubra as possíveis causas da dor de cabeça do lado direito, incluindo tensão muscular, problemas sinusais e enxaquecas. Nosso guia abrangente oferece insights sobre gatilhos comuns, impactos do estresse e condições graves a serem observadas. Aprenda quando buscar ajuda médica e explore opções de manejo efetivas e remédios caseiros para aliviar o desconforto. Entenda como medidas de saúde proativas, como consultar um profissional de saúde, podem ajudar a abordar causas subjacentes, garantindo um recurso único para aqueles que buscam alívio da dor de cabeça do lado direito.
Jan 13, 2025
Entendendo a Dor de Cabeça do Lado Direito e Sua GestãoExplore os gatilhos e sintomas comuns da dor de cabeça do lado direito, incluindo tensão, fatores dietéticos e influências ambientais. Descubra as condições médicas subjacentes associadas a essa dor, como enxaquecas e infecções sinusais, e aprenda quando buscar atendimento de emergência. Nosso guia abrangente descreve estratégias eficazes de gerenciamento, incluindo mudanças no estilo de vida, técnicas de redução do estresse e opções de tratamento médico. Capacite-se com o conhecimento sobre como identificar gatilhos e implementar estratégias de prevenção a longo prazo para melhorar sua qualidade de vida. Visite-nos para obter insights sobre o diagnóstico e tratamento da dor de cabeça do lado direito.
Jan 19, 2025
Entendendo a Fisiologia da Tensão Muscular e das CefaleiasDescrição: Descubra a intrincada relação entre a tensão muscular e as cefaleias em nosso guia abrangente. Aprenda como o estresse, a má postura e as escolhas de estilo de vida contribuem para a rigidez muscular e as dores de cabeça tensionais. Explore abordagens de tratamento eficazes, incluindo terapias físicas, técnicas de relaxamento e métodos integrativos que combinam práticas convencionais e holísticas. Encontre soluções práticas para aliviar a tensão muscular, gerenciar os sintomas de dor de cabeça e melhorar seu bem-estar geral. Diga adeus às dores de cabeça crônicas e abrace um estilo de vida mais saudável.
Feb 25, 2025
Dor de cabeça ao caminhar: Causas e opções de alívio
May 01, 2025
Descubra estratégias eficazes para gerenciar enxaquecas, compreendendo e identificando seus gatilhos. Este guia abrangente mergulha nos aspectos neurológicos das enxaquecas, ajudando você a reconhecer gatilhos comuns e menos óbvios.
May 24, 2025
Cefaleias de Abstinência de Cafeína: Como Lidar
Jun 03, 2025
Como aprender seus gatilhos fortalece as escolhas diárias
Jul 03, 2025
Compreendendo os Triptans: Tratamento Agudo de Enxaqueca Explicado
Jul 06, 2025