Neuroscience
Medical_treatment
Brain Stimulation
Nervous System
Physiology
HTML
CSS
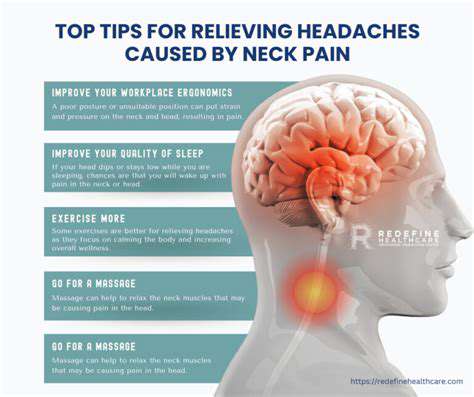
Headaches
Pain Management
片頭痛治療のための神経調節デバイスの比較
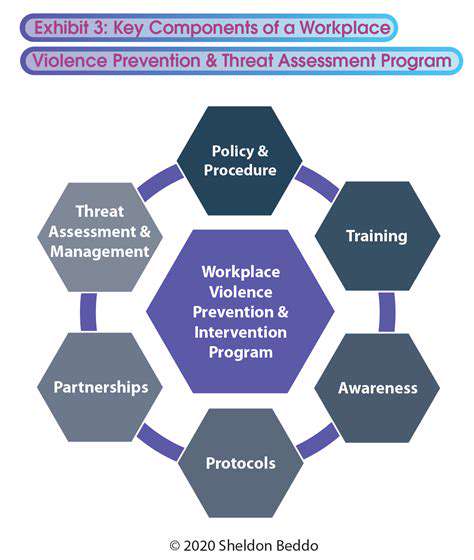
広範な概要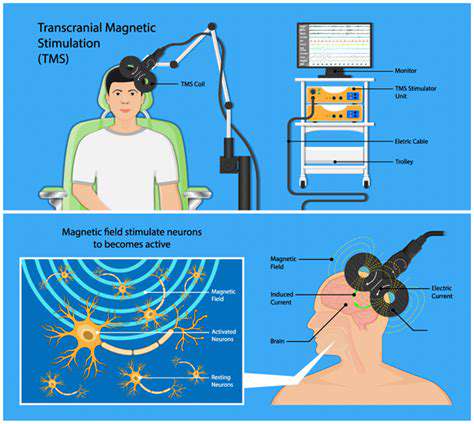

神経調節は魅力的な分野です。脳や体内の神経回路の活動を変化させることを目的としたさまざまな技術が含まれています。この洗練されたアプローチは、幅広い症状の非侵襲的または最小限の侵襲的な治療法を提供します。
片頭磁気刺激 (TMS) による片頭痛予防
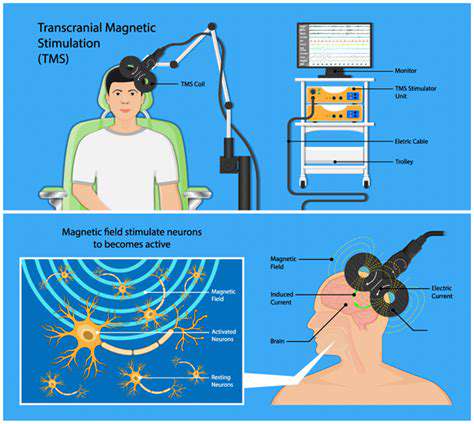
片頭磁気刺激 (TMS) の原理
頭蓋骨を介して脳に磁気パルスを送り込むことで、脳の特定の領域に刺激を与える治療法です。
慢性頭痛管理のための迷走神経刺激 (VNS)

迷走神経について
咳をする際に頭痛がする時の情報迷走神経は、脳幹から体幹にかけて広がる重要な神経です。それは、心臓、肺、消化器系など多くの臓器に接続し、自律神経系の重要な役割を果たしています。迷走神経は、体の様々な機能を調整し、バランスを保つ上で不可欠な働きをしています。慢性頭痛の治療において、迷走神経刺激療法は、神経系の活動に影響を与え、頭痛の発生や頻度を軽減する可能性があります。
片頭痛誘発痛に対する末梢神経刺激
片頭痛の誘因を理解する
片頭痛患者はしばしば、激しい頭痛を引き起こす可能性のある複雑な要因の相互作用を経験します。これらの誘因を特定することは、頭痛を軽減するために非常に重要です。
Read more about 片頭痛治療のための神経調節デバイスの比較
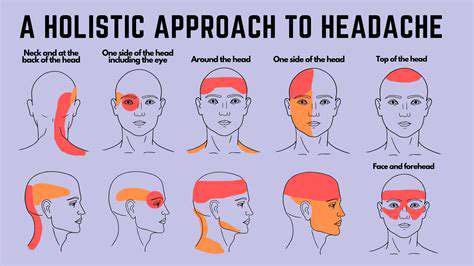
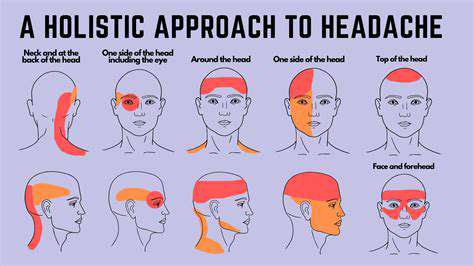
症状、原因、治療頭皮痛は鈍い痛みから鋭い刺すような感覚まで幅広く、日常生活や全体的な健康に影響を与えます。圧痛や伴う頭痛などの症状を早期に認識することが、効果的な管理には不可欠です。頭皮痛の潜在的な原因は、緊張性頭痛、乾癬などの頭皮の状態、後頭神経痛などの神経の問題まで多岐にわたります。効果的な治療戦略には、一般用鎮痛薬、炎症用の局所薬、持続的な問題に対する専門的な相談が含まれます。この包括的なガイドは、一般的な症状、潜在的な原因、治療の選択肢を概説し、個人が頭皮痛を効果的に管理するのを助けます。ストレス管理技術、栄養価の高い食事、医療提供者との定期的なチェックインを含む、頭皮の健康を維持するためのホリスティックなアプローチを探求してください。頭皮の健康を優先することで、痛みのない活力に満ちた生活を実現できます。
Nov 12, 2024
頭皮の痛みの一般的な原因を理解し、効果的な治療オプションを探ります。私たちの包括的なガイドでは、片頭痛や緊張型頭痛から、乾癬や神経に関連する痛みのような頭皮の状態まで、すべてをカバーしています。症状を認識することの重要性、基礎的な病状の管理、および不快感を和らげるための薬と家庭療法の活用について学びましょう。ライフスタイルの変更でウェルビーイングを向上させ、頭皮の健康に合わせた解決策を見つけてください。今すぐ情報を得て、持続的な頭皮の痛みから解放されましょう!
Nov 22, 2024
痛みの結び目に関する当社の啓発的な記事では、ストレス、トラウマ、および身体の痛みの間の複雑な関係を探ります。感情的ストレスが筋肉の緊張を引き起こし、不快感をもたらす仕組みを学び、マインドフルネス、マッサージ療法、身体的実践などの効果的な緩和戦略を発見します。痛みの結び目の症状と原因を特定する方法についての洞察を得て、専門家の助けが必要なタイミングを理解します。実践的な技術と長期的な解決策を通じて、健康な心と身体のつながりを育成し、痛みのサイクルを克服できるよう自分を Empower してください。不快感の背後にある感情的な要素を解きほぐし、ウェルネスへのホリスティックなアプローチを受け入れましょう。
Dec 07, 2024
痛みは神経、血管、筋肉、副鼻腔、または顎の問題に起因する可能性があります。- 症状の特定:症状には、拍動性の痛み、光に対する過敏、悪心、および視覚の障害が含まれます。症状日記の保持は診断に役立ちます。- 治療選択肢:治療は原因に基づき異なり、一般用医薬品、ライフスタイルの変更、そして鍼治療などの代替療法を含む場合があります。症状と種類- 一般的な症状:鈍痛、鋭い痛み、拍動感、圧迫感。伴う症状として、光や音に対する過敏性が含まれる場合があります。- 偏頭痛と頭痛:偏頭痛は右側頭痛の主要な原因であり、光に対する敏感さと悪心を伴います。他のタイプには、緊張性頭痛や群発頭痛があります。管理戦略- 自宅療法:冷湿布や一般用医薬品は即効性の緩和を提供できます。水分補給、食事、睡眠に焦点を当てたライフスタイルの変更は予防にとって重要です。- 専門医療:持続する痛みの場合は、専門の医療提供者に相談することが不可欠です。専門的な治療には、処方薬、理学療法、または認知行動療法が含まれる場合があります。結論:右側頭痛の原因、症状、治療選択肢を理解することは、効果的な管理に不可欠です。早期の介入は生活の質を向上させ、不快感を減少させる可能性があります。個別のケアについては、必ず医療提供者に相談してください。詳細な情報を得るには、右側頭痛に関する私たちの詳細な記事を参照してください。
Jan 13, 2025
右側の頭痛の原因と管理方法を探求します。筋肉の緊張、副鼻腔の問題、偏頭痛などの潜在的な原因を知りましょう。私たちの包括的なガイドは、一般的な引き金、ストレスの影響、注意すべき深刻な状態についての洞察を提供します。医学的な注意を求めるべきタイミングを学び、快適さを軽減するための効果的な管理オプションや家庭療法を探ります。医療専門家に相談するなどの積極的な健康対策が根本的な原因に対処するのにどのように役立つかを理解し、右側の頭痛からの緩和を求める人々のためのワンストップリソースを提供します。
Jan 13, 2025
右側の頭痛とその管理を理解する右側の頭痛の一般的な引き金と症状を探ります。緊張、食事要因、環境的影響が含まれます。この痛みに関連する基礎的な医学的状態(片頭痛や副鼻腔感染症など)を発見し、いつ緊急治療を受けるべきかを学びます。私たちの包括的なガイドは、ライフスタイルの変更、ストレス軽減技術、医療治療の選択肢など、効果的な管理戦略を概説しています。引き金を特定し、生活の質を向上させるための長期的な予防戦略を実施する知識を身につけましょう。右側の頭痛の診断と治療に関する洞察を得るために、ぜひお越しください。
Jan 19, 2025
筋肉の緊張と頭痛の生理学の理解説明:私たちの包括的なガイドで、筋肉の緊張と頭痛の複雑な関係を発見します。ストレス、不良姿勢、生活習慣の選択が筋肉の緊張と緊張型頭痛にどのように寄与するかを学びます。物理療法、リラクゼーション技術、そして従来の方法とホリスティックな実践を組み合わせた統合的なアプローチなど、効果的な治療法を探ります。筋肉の緊張を和らげ、頭痛の症状を管理し、全体的な健康を向上させる実用的な解決策を見つけます。慢性的な頭痛にさよならを告げ、より健康的なライフスタイルを迎え入れましょう。
Feb 25, 2025
片頭痛の引き金を理解し特定することで、片頭痛を効果的に管理するための戦略を発見します。この包括的なガイドは、片頭痛の神経学的側面を深く掘り下げ、一般的な引き金とそうでない引き金を認識するのに役立ちます。
May 24, 2025