Migraine Myths Debunked: Separating Fact from Fiction
Myth 2: Stress and Anxiety are the Sole Culprits
Stress and Anxiety's Role: A Nuance
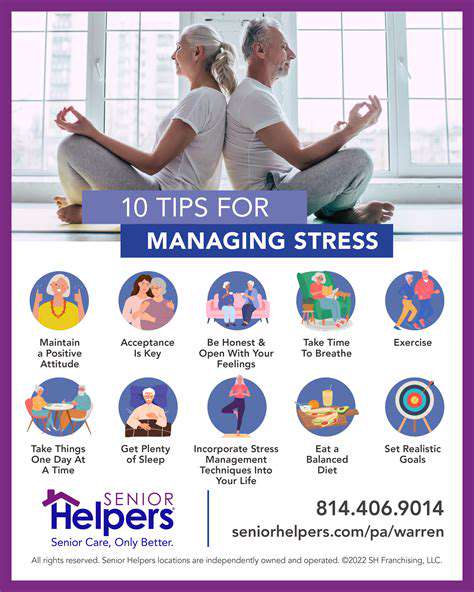
While stress and anxiety can certainly trigger migraines, painting them as the sole culprits oversimplifies a complex neurological condition. Numerous studies suggest a correlation, but not a direct causality. understanding the interplay between emotional factors, environmental triggers, and individual physiological responses is crucial to effective migraine management.
Focusing solely on stress management might not address the underlying mechanisms contributing to migraine attacks in every individual. A holistic approach encompassing various lifestyle factors, including sleep, diet, and hydration, is often more effective in preventing and treating migraines.
Dietary Triggers: Beyond the Obvious
The connection between certain foods and migraine attacks is well-documented, yet the specific mechanisms and individual sensitivities vary significantly. While chocolate and aged cheeses are frequently cited, the triggers extend to a wider range of dietary components, including processed foods, caffeine fluctuations, and even specific types of fruits and vegetables.
Recognizing personal dietary triggers requires careful observation and meticulous logging of food intake in relation to migraine attacks. This detailed approach can reveal subtle patterns and help individuals identify and avoid specific dietary culprits.
Sleep Disruptions: A Critical Link
Sleep disturbances, both insufficient sleep and poor sleep quality, are strongly implicated in migraine development. The impact of inadequate rest on the body's natural regulatory processes can contribute to heightened sensitivity to various triggers, making individuals more susceptible to migraine attacks.
Addressing sleep hygiene, such as establishing a regular sleep schedule, creating a conducive sleep environment, and managing stress before bed, can significantly improve sleep quality and potentially reduce the frequency and severity of migraine attacks.
Environmental Factors: Unseen Influences
Environmental factors, including changes in weather patterns, barometric pressure fluctuations, and even certain scents, can act as potent migraine triggers. These triggers often operate subtly, making them difficult to identify and manage, yet their impact on migraine sufferers can be substantial.
Understanding personal sensitivities to environmental factors requires detailed observation and documentation of environmental conditions in relation to migraine attacks. This data can help identify specific environmental triggers and inform strategies for avoidance or mitigation.
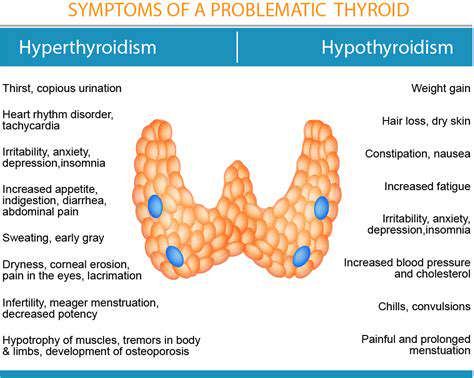
Hormonal Influences: A Significant Factor
Fluctuations in hormone levels, particularly in women, are a well-recognized factor in migraine susceptibility. Hormonal changes associated with menstruation, pregnancy, and menopause can trigger or exacerbate migraine attacks in many individuals.
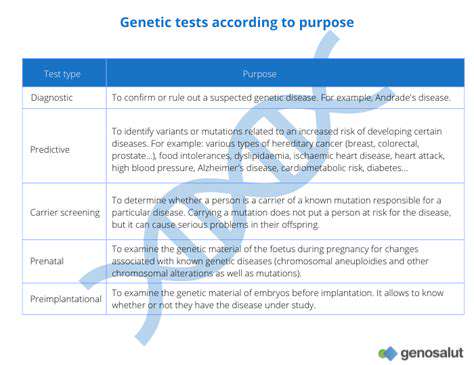
Genetic Predisposition: An Often Overlooked Aspect
A significant portion of migraine sufferers have a family history of the condition, suggesting a genetic component. While genetic predisposition doesn't dictate an inevitable diagnosis, it highlights the importance of understanding individual vulnerability and the role of inherited factors in migraine development.
This understanding can guide preventive measures and personalized treatment strategies to manage migraine attacks effectively.
Myth 3: Migraines Only Affect Women
Myth Debunked: Migraines Affect Both Genders
The notion that migraines primarily affect women is a persistent myth that needs to be addressed. While it's true that women experience migraines more frequently than men, this doesn't negate the significant impact migraines have on men's lives. Men often face challenges in getting their migraine pain recognized and treated effectively, leading to delays in diagnosis and management. This often stems from societal expectations that men should be stoic and suppress pain, further compounding the problem. Understanding that migraines can affect anyone, regardless of gender, is crucial for fostering a more supportive and effective approach to diagnosis and treatment.
Research consistently highlights a notable difference in the prevalence of migraines between men and women. While women experience migraines more frequently, this doesn't diminish the validity of men's experiences. Men who experience migraines often face skepticism and delayed diagnosis due to societal biases. This underscores the need for greater awareness and understanding of migraine symptoms in both genders.
Underlying Biological Factors in Migraine Prevalence
While the exact reasons for the gender disparity in migraine prevalence are still under investigation, several biological factors are suspected to play a role. Hormonal fluctuations in women, particularly estrogen levels, are thought to contribute to the heightened susceptibility. However, this isn't the sole determinant, and men experience migraines due to a complex interplay of genetic predispositions, environmental triggers, and other biological factors. Further research is needed to fully understand the intricate mechanisms underlying migraine development in both genders.
Beyond hormonal influences, genetic factors and other biological variations between genders likely contribute to the observed difference in migraine prevalence. Neurological pathways and the specific responses to pain stimuli may also differ between men and women, impacting migraine experiences. Investigating these biological nuances is vital for improving diagnostic accuracy and developing targeted treatments for both genders.
Impact on Men's Health and Well-being
The societal perception of migraines as a women's problem can significantly impact men's health and well-being. Men often experience difficulties in getting their migraine pain recognized and treated effectively, which can lead to a diminished quality of life. The stigma associated with migraine can also affect men's mental health, potentially leading to feelings of isolation, frustration, and even depression. It's crucial to recognize that migraines affect men profoundly, requiring a compassionate and understanding approach to diagnosis, treatment, and support.
The impact of undiagnosed and untreated migraines on men's lives is substantial. Missed work, decreased productivity, and strained relationships are just some of the repercussions that can arise. Promoting awareness and education about migraines in men is essential for ensuring they receive the appropriate care and support they need. Encouraging open communication about migraine experiences is also crucial for fostering a more supportive environment.