Gestion de la douleur de tête avec des affections coexistantes (p. ex., fibromyalgie, IBS)
L'interaction complexe entre les maux de tête et les affections chroniques

Comprendre les déclencheurs
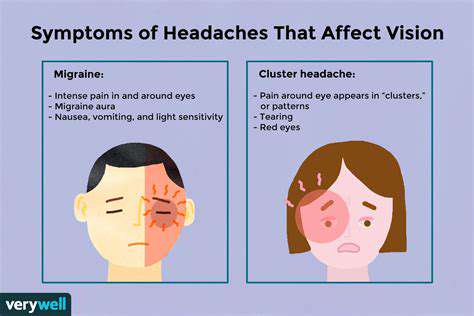
Les maux de tête touchent des millions de personnes dans le monde, avec des déclencheurs allant de l'environnement
Identification des déclencheurs potentiels de maux de tête dans les affections coexistantes
Identification des maux de tête liés au stress
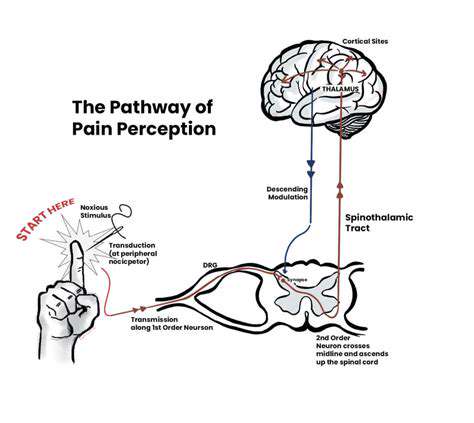
Le stress chronique active l'axe hypothalamo-hypophyso-surrénalien, créant des changements physiologiques qui précipitent les maux de tête. M
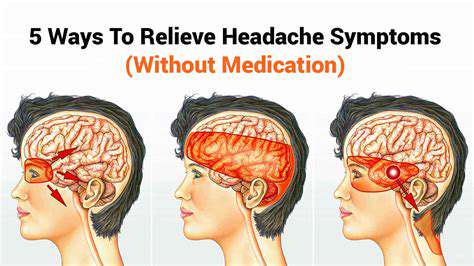
Ajustements du style de vie pour soulager les maux de tête à long terme

Prioriser le sommeil
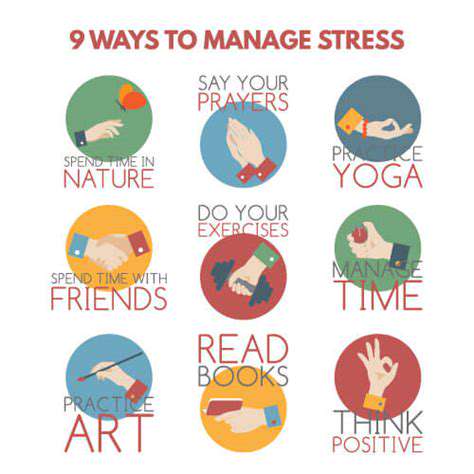
Gestion du Stress
Alimentation et Hydratation
Une alimentation équilibrée et une bonne hydratation sont essentielles pour le bien-être général et la prévention des maux de tête. Il est important de consommer des aliments nutritifs et de rester hydraté, en buvant suffisamment d'eau tout au long de la journée. Certaines habitudes alimentaires peuvent déclencher des maux de tête, comme une consommation excessive de caféine ou d'alcool. Il est recommandé d'identifier ces déclencheurs et de les éviter pour prévenir les maux de tête.
Environnement de Travail et de Vie
L'environnement de travail et de vie peut jouer un rôle dans la fréquence des maux de tête. Un environnement bruyant, une mauvaise posture prolongée ou une exposition excessive à la lumière peuvent contribuer à des céphalées. Il est important d'adapter son environnement pour minimiser ces facteurs déclencheurs et maintenir un espace de vie et de travail confortable. Des pauses régulières, une bonne posture et un éclairage adéquat peuvent faire la différence.